WSC 23-24 Conference 9, Case 3
Signalment:
4-year-old, Angus cow, bovine (Bos taurus)
History:
Four adult Angus cows and an adult Hereford bull died suddenly a few days after being moved to lush pasture.
Gross Pathology:
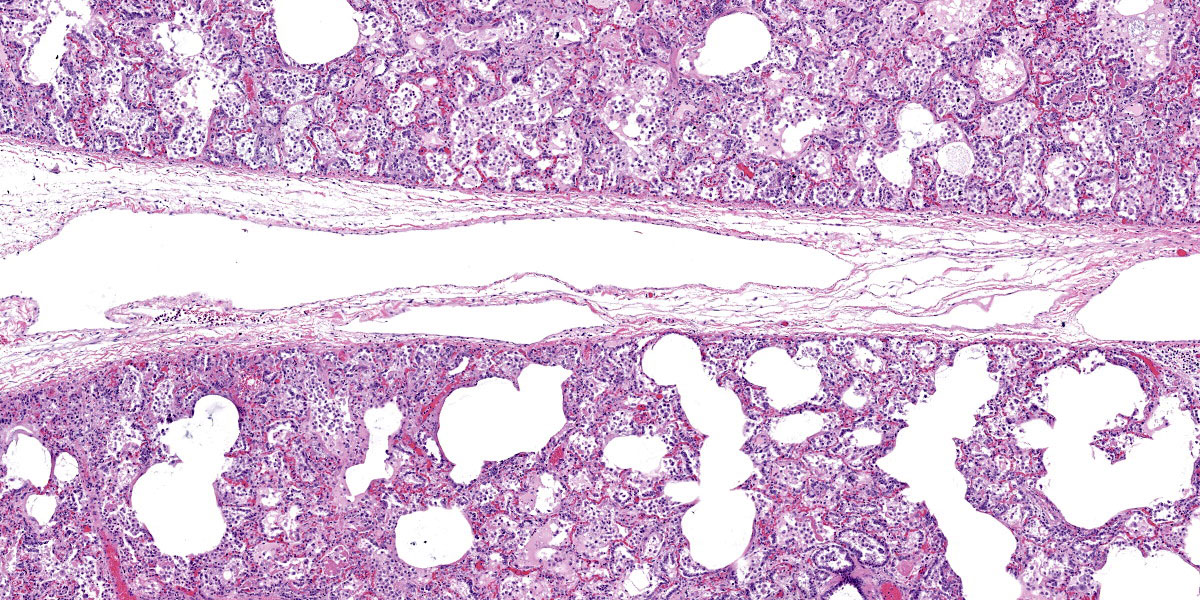
The lungs did not collapse when the thorax was opened. The majority of the lung parenchyma was red, heavy, wet and meaty with emphysema and edema in the interlobular septa and moderate numbers of petechiae on the surface. Approximately 10-30% of the lung parenchyma in the cranioventral lung fields was dark red to plum colored, firm and consolidated.
Laboratory Results:
Pasteurella multocida was isolated on bacterial culture of the consolidated lung.
PCR testing of the lung was negative for bovine viral diarrhea (BVD) virus, bovine herpesvirus-1 (IBR), bovine respiratory syncytial virus (BRSV), Mycoplasma bovis, bovine respiratory coronavirus, and bovine influenza virus (BIV).
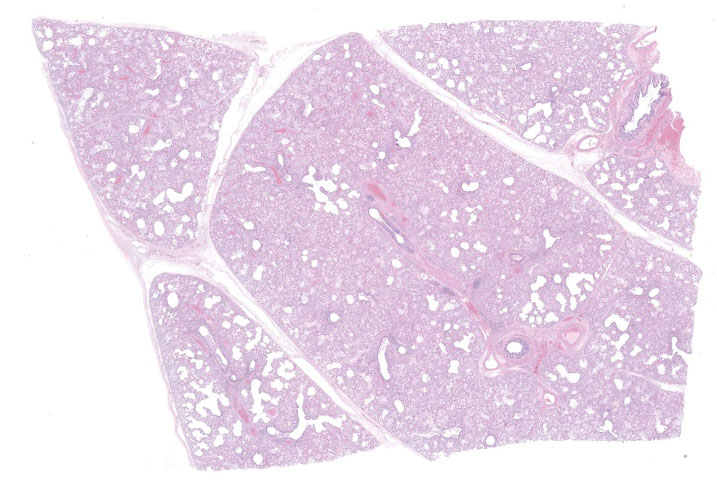
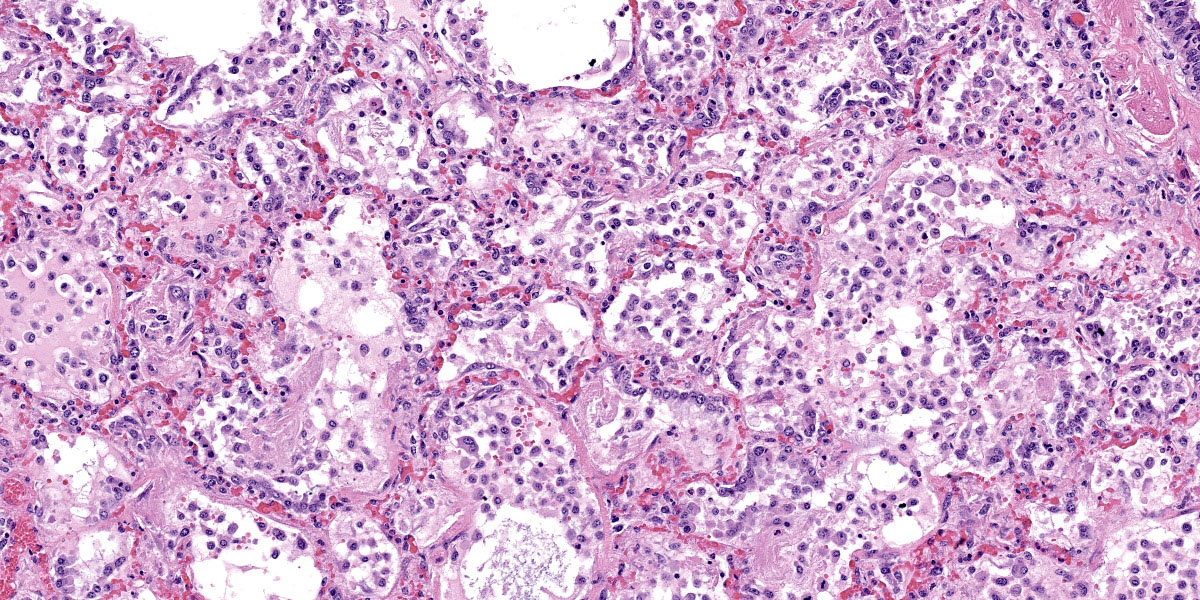
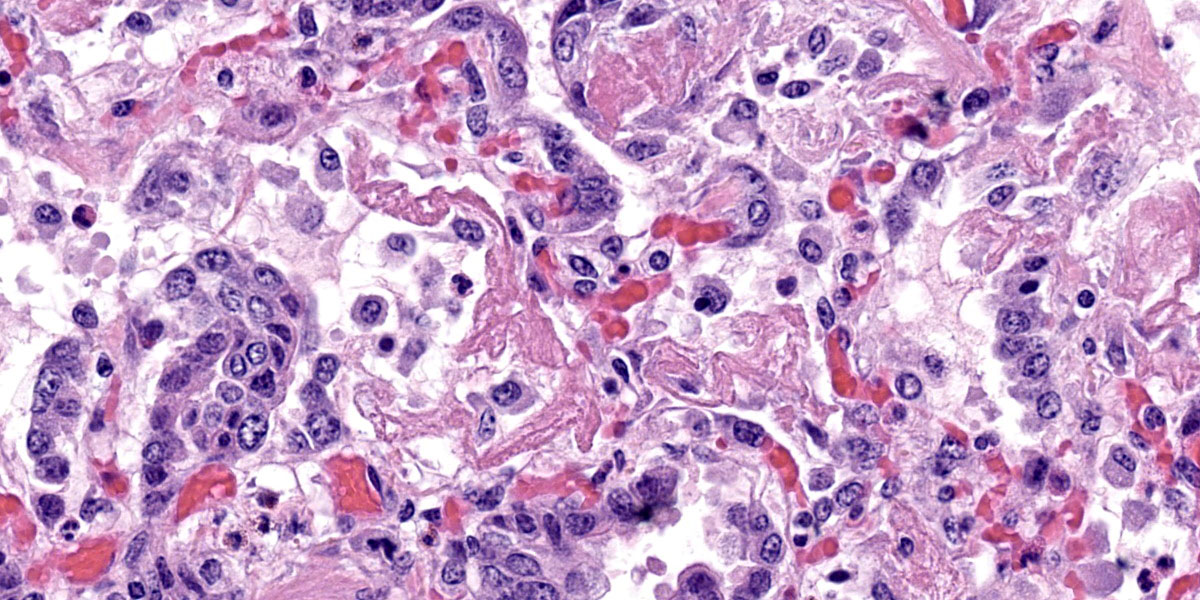
Microscopic Description:
The lung is diffusely congested. In the majority of the lung, the alveoli are filled with edema and fibrin mixed with variable numbers of macrophages, small numbers of neutrophils and rare multinucleated giant cells. The fibrin occasionally forms hyaline membranes that are associated with the alveolar wall. The alveolar septa are thickened by fibrin, edema, macrophages, lymphocytes and swollen type II pneumocytes that epithelialize the alveolar wall. The interlobular septa and pleura are thickened by edema and emphysema.
Contributor’s Morphologic Diagnosis:
Lung: Interstitial pneumonia, acute, diffuse, severe, with hyaline membrane formation, type II pneumocyte hyperplasia, edema, and emphysema (acute bovine pulmonary edema and emphysema)
Contributor’s Comment:
The clinical history and the gross and microscopic lesions are consistent with the respiratory disease known as acute bovine pulmonary edema and emphysema (ABPEE). ABPEE is a toxic interstitial pneumonia of cattle.3,5 The disease most commonly occurs in adult cattle.
Calves appear to be resistant to the disease. ABPEE typically occurs in the fall 4-10 days after cattle are moved from summer pastures to lusher fall pastures, but it can occur any time of the year when cattle are moved to lush pastures.
ABPEE is caused by L-tryptophan within plants being converted to 3-methylindole by rumen microbes.1,2,3,5,6,7 The 3-methylindole formed in the rumen is absorbed into the bloodstream, eventually making it to the lungs.3,5 There is evidence that suggests 3-methylindole preferentially binds in the lung of susceptible species compared to other organs such as the liver.7 Within the lung, 3-methylindole is converted to unknown toxic metabolites by mixed function oxidases, mainly cytochrome p450 in the nonciliated bronchiolar epithelial cells.3,5 The toxic metabolite of 3-methylindole causes necrosis of bronchial epithelium and type I pneumocytes, endothelial cell swelling, and increased vascular permeability. The increase in vascular permeability leads to edema and thickening of the alveolar wall. Type II pneumocyte hyperplasia occurs in response to necrosis of type I pneumocytes.
Typical gross lesions of ABPEE in cattle include pale to red, edematous, meaty and rubbery lungs that fail to collapse when the thorax is opened.3,5 The lungs are often emphysematous. Microscopically, there is interstitial and alveolar edema with hyaline membrane formation in alveoli. There is often interstitial emphysema. Eosinophils and neutrophils may be present within alveolar septa. In more chronic cases, there is diffuse type II pneumocyte hyperplasia and alveolar fibrosis. Secondary suppurative bronchopneumonia can occur. Differential diagnoses include 4-ipomeanol from ingestion of Fusarium solani-contaminated sweet potatoes, ingestion of purple mint (Perilla frutescens), ingestion of rapeseed and kale (Brassica species), ingestion of stinkwood (Zieria arborescens), extrinsic allergic alveolitis, hypersensitivity to Dictyocaulus larvae, and viral pneumonia, particularly that caused by BRSV.
Contributing Institution:
New Mexico Department of Agriculture
Veterinary Diagnostic Services
www.nmda.nmsu.edu/vds
JPC Diagnosis:
Lung: Pneumonia, interstitial, diffuse, severe, with septal necrosis, marked alveolar and interlobular edema, hyaline membranes, and type II pneumocyte hyperplasia.
JPC Comment:
3-methylindole (3-MI) toxicity is a prime example of biotransformation gone bad. Biotransformation refers to metabolic reactions that generally serve to increase the water solubility of compounds and thus enhance their excretion.4 These reactions transform toxic compounds into benign metabolites and are also critical to the metabolism of endogenous compounds such as cholesterol, steroids, vitamin D, bile acids, and fatty acids.4 In some instance, however, biotransformation may form reactive intermediates, such as electrophiles and free radicals, that are directly toxic or mutagenic.4
Biotransformation is typically described as a phased process, with Phase I reactions consisting primarily of oxidation, reduction, and hydrolytic reactions that cause small changes in the water solubility of the compound.4 It is the subsequent Phase II reactions where large changes in water solubility are effected, typically via conjugation reactions where a variety of hydrophilic moieties are added to the subject compound.4 Phase III, the final phase of biotransformation, refers to the transporter-mediated efflux of the metabolite for excretion.
Phase I metabolism is carried out largely through a family of heme-containing enzymes referred to as cytochrome P450s (CYPs). Given its major role in detoxification, the liver expresses high levels of a variety of CYPs located in the smooth endoplasmic reticulum of hepatocytes.4 In all species, CYPs are more highly expressed in centrilobular zone hepatocytes, leading to centrilobular necrosis when biotransformation creates toxic intermediates. CYPs are not restricted to the liver but are found in a variety of tissues throughout the body. In the lung, CYP2F enzymes are abundant, particularly in the club cells, the nonciliated bronchiolar epithelial cells formerly called Clara cells.4
Phase II biotransformation reactions are primarily conjugation reactions that occur in the cytosol. These reactions include glucuronidation, sulfation, and glutathione conjugation, along with less common reactions such as methylation, acetylation, and amino acid conjugation.4 There are significant species differences in which reactions predominant, particularly with glucuronidation and sulfation reactions. Glucuronidation is the major Phase II metabolic pathway in all mammalian species except for cats, who assert their feline singularity by preferentially using sulfation reactions.4
As the contributor notes, the critical step in the pathogenesis of ABPEE is the biotransformation of 3-MI, a relatively inert compound, to a toxic electrophilic intermediate by CYPs in the lung. The resulting toxic intermediate alkylates cellular macromolecules, resulting in lipid peroxidation, membrane damage, and the subsequent necrosis of bronchiolar epithelial cells and type I pneumnocytes.3 Type II pneumocytes are relatively unaffected despite their high CYP activity due to their high levels of glutathione and phase II enzymes which are thought to protect them from injury.3 In fact, type II pneumocyte hyperplasia, not necrosis, is a characteristic histologic change of ABPEE as type II pneumocytes proliferate to repair the extensively damage alveolar epithelium.
Dr. Williams felt that this case was a great, straightforward example of atypical interstitial pneumonia in cattle. He noted areas within the lung where the alveolar type I pneumocytes appeared to be replaced with bronchiolar epithelium, a metaplastic change referred to as bronchiolarization or Lambertosis. This change occurs when bronchiolar epithelium attempts to repair alveolar damage by growing out from the bronchioles and into the alveolar sacs and occurs with severe diffuse alveolar damage.
Dr. Williams also noted what appear as undulating nodules of smooth muscle in the wall of the pulmonary vein. This represents a normal spiral of smooth muscle present normally in the pulmonary veins of bovids and should not be confused with hypertensive or neoplastic change. Finally, Dr. Williams noted that edema fluid can drain through lymphatic slits present around the bronchovascular bundle, making this a good location to find siderophages if you suspect heart failure.
Dr. Williams discussed the edema and emphysema noted by the contributor. While the interlobular septa are markedly expanded by clear space, on the examined slide, these spaces appeared largely to be lymphatic channels filled with edema fluid. Dr.Williams interpreted the remaining clear spaces within the pulmonary parenchyma to be alveolar ducts rather than discontinuous alveolar septa. The JPC morphologic diagnosis reflects these interpretations, arrived at after much discussion.
References:
- Bray TM, Emmerson KS. Putative mechanisms of toxicity of 3-methylindole: from free radical to pneumotoxicosis. Annu Rev Pharmacol Toxicol. 1994;34: 91-115.
- Carlson JR, Yokoyama MT, Dickinson EO. Induction of pulmonary edema and emphysema in cattle and goats with 3-methylindole. Science. 1972; 176(4032): 298-299.
- Caswell JL, Williams KJ. Respiratory system. In: Maxie G, ed. Jubb, Kennedy, and Palmer’s Pathology of Domestic Animals. 6th Vol 2. Elsevier;2016:465-591.
- Lehman-McKeeman LD, Armstrong LE. Biochemical and molecular basis of toxicity. In: Haschek WM, Rousseaux CG, Wallig MA, et al., eds. Haschek and Rousseaux’s Handbook of Toxicologic Pathology. Academic Press;2022: 24-30.
- Lopez A, Martinson SA. Respiratory system, mediastinum, and pleura. In: Zachary JF, ed. Pathologic Basis of Veterinary Disease. 6th ed. Elsevier;2017:471-560.
- Schiefer B, Jayasekara MU, Mills JHL. Comparison of naturally occurring and tryptophan-induced bovine atypical interstitial pneumonia. Vet Pathol. 1974; 11 (4):327-339.
- Yost GS. Mechanisms of 3-methylindole pneumotoxicity. Chem Res Toxicol.1989; 2(5):273-279.