Signalment:
16-month-old intact mixed breed male cat,
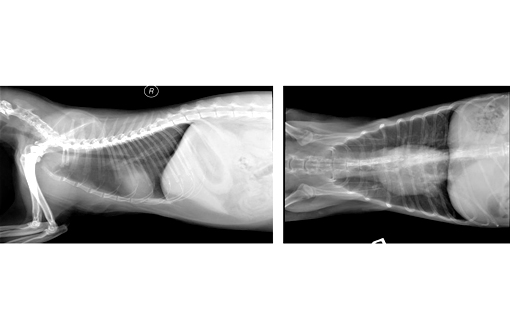
Felis cats.The animal was a rescue shelter cat current on all vaccinations. The animal presented with dyspnea and strider upon exercise. Radiographs of the lungs revealed a diffuse interstitial pattern.
Gross Description:
The carcass demonstrated an adequate nutritional plane. There was a red watery discharge from both nostrils. Upon reflecting the skin, the subcutaneous tissues were noted to stick to the prosectors gloves. The lungs did not collapse upon opening the thoracic cavity. They were moist and diffusely mottled gray to pink. Approximately 3mls of a pink watery fluid was in the chest cavity. The heart was enlarged and occupied three and a half intercostal spaces. A small amount of fluid oozed form a cut surface of the lungs.
Histopathologic Description:
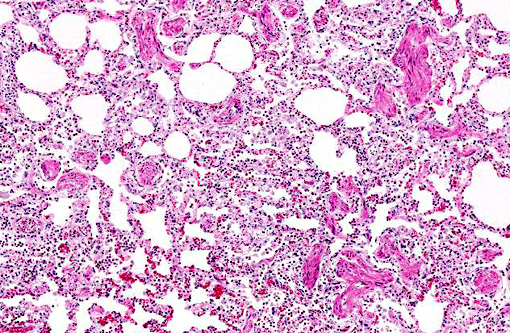
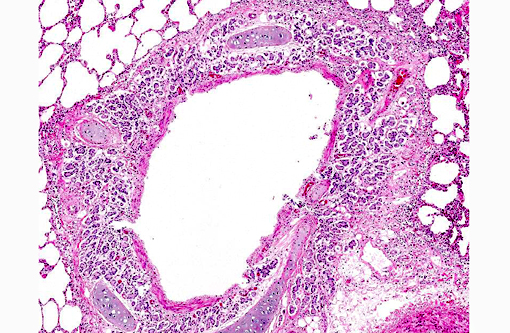
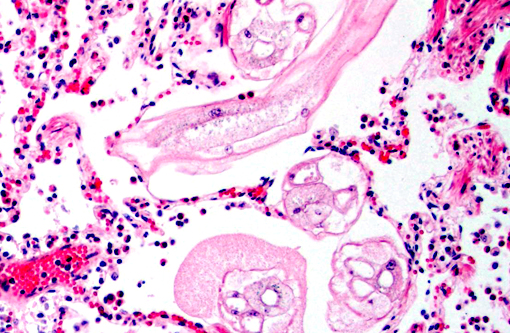
There is moderate to marked hyperplasia and hypertrophy of the tunica muscularis of pulmonary arteries. The smooth muscle of bronchioles and alveolar ducts is also prominent. The epithelial linings of many bronchi are sloughed and there are increased numbers of bronchial glands. Small to moderate numbers of lymphocytes, plasma cells and macrophages infiltrate bronchial and bronchiolar walls, peribronchial connective tissue, and adjacent periarterial tissue. Peribronchial stroma is expanded by small clear spaces (edema).
Morphologic Diagnosis:
Bronchitis and bronchiolitis, chronic, multifocal, moderate, with alveolar ductal and arterial smooth muscle hyperplasia, and peribronchial glandular hyperplasia, lung.
Lab Results:
| RBC | 8.69 M/u/L |
| HGB | 11.9 g/Dl |
| HCT | 40.7% |
| MCV | 46.9 fl |
| MCH | 13.7 pg |
| WBC: | 10.8 K/ul |
| NEU: | 3.47 32.2%N |
| LYM: | 5.69 52.9%L |
| MONO: | 0.026 0.239%M |
| EOS | 1.57 14.6%E |
| BASO | 0.002 0.020 %B |
Condition:
Feline allergic airway disease
Contributor Comment:
Based on the microscopic lesions, a diagnosis of feline asthma syndrome (FAS) was made. This syndrome is characterized by episodes of coughing, wheezing and or dyspnea which are due to the bronchoconstriction secondary to hyperactivity of airway smooth muscle.(1) It has been referred to as allergic bronchitis or allergic pneumonia. Though the exact cause is unknown, it is associated with a type I immediate hypersensitivity reaction to inhaled antigens. Inhaled cat litter dust, aerosol sprays and cigarette smoke as well as infectious causes have been associated with this syndrome.(3) This disease is rarely the primary cause of death except when a secondary bacterial pneumonia occurs.
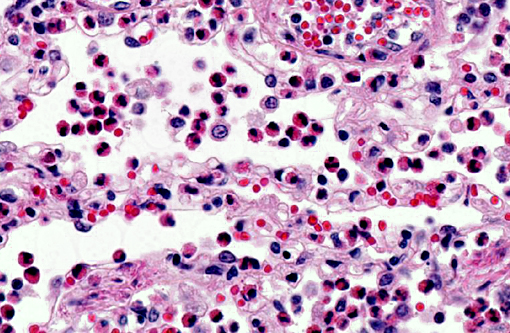
In the early stages of this disease there is a mild eosinophilic inflammatory infiltrate with mucosal edema.(3) As seen in this case, eosinophils are not always the prominent cell type. In the more advanced stages the characteristic lesions include bronchial gland hyperplasia along with smooth muscle hypertrophy of arteries and airways.
JPC Diagnosis:
Lung: Pneumonia, eosinophilic, chronic, multifocal, moderate with bronchiolar and smooth muscle hyperplasia, and intrabronchiolar adult nematodes.
Conference Comment:
This is an interesting case, not in its classic or dramatic presentation of a lesion as often observed in WSC cases, but rather in its subtlety, effectively delivering a real-world diagnostic challenge to all conference participants. The contributors diagnosis of feline asthma is based on the presence of smooth muscle and peribronchial gland hyperplasia as corresponding with the animals clinical signs, as well as a diffuse mild eosinophilic infiltrate, primarily within alveoli. However, a number of slides contain tangential sections of degenerate adult nematodes which were not described by the contributor, and which we believe are a primary component of this clinical presentation. The level of degeneration precludes definitive diagnosis; however, a large, multinucleated intestine is present in some nematode sections and when coupled with the vague coelomyarian musculature, strongly suggests a metastrongyle.
Aelurostrongylus abstrusus is considered a ubiquitous nematode of domestic cats and thus the most likely species of metastrongyle in this case.(3) Another possibility is the feline parasite
Ollulanus tricuspis, a trichostrongyle which could have been regurgitated and aspirated into the lung parenchyma.
The changes seen in this case correlate best with a late-stage chronic infection with
A. abstrusus in cats. In one study, 24 weeks following infection, eggs and larvae were completely absent and adult nematodes present in only 3 of nearly 100 examined histologic sections.(2) Smooth muscle and peribronchial gland hyperplasia are typical findings in these cases, though it is worth mentioning this is often considered a normal finding in healthy cats with no evidence of parasitism.(1)
A. abstrusus is common in cats, with an array of corresponding clinical signs from asymptomatic to chronic coughing and tachypnea. In characteristic lesions, there are nodules formed by masses of eggs and larvae in alveoli and terminal bronchioles with few adult worms. Eosinophils and neutrophils predominate early, with more mononuclear cells and giant cells occurring later. Typically, chronic cases devoid of larvae and eggs have remaining epithelialized alveoli and septa thickened by fibrous tissue and smooth muscle.(1) The infection is usually self-limiting(3) and given the mild extent of pathology in most slides, it is possible there were unidentified contributing factors to the clinical presentation described in this case.
References:
1. Caswell JL, Williams KW. Respiratory system. In: Maxie MG, ed. Jubb, Kennedy, Palmers Pathology of Domestic Animals. 5th ed. Vol. 2. Philadelphia, PA: Elsevier Saunders; 2007:557, 649-650.
2. Hamilton JM. Experimental lungworm disease of the cat. J Comp Pathol. 1966;76:147-157.
3. Lacorcia L, Gasser RB, Anderson GA, Beveridge I. Comparison of bronchioalveolar lavage fluid examination and other diagnostic techniques with the Baermann technique for detection of naturally occurring Aelurostrongylus abstrusus infection in cats. JAVMA. 2009;235(1):43-49.