Signalment:
Gross Description:
Histopathologic Description:
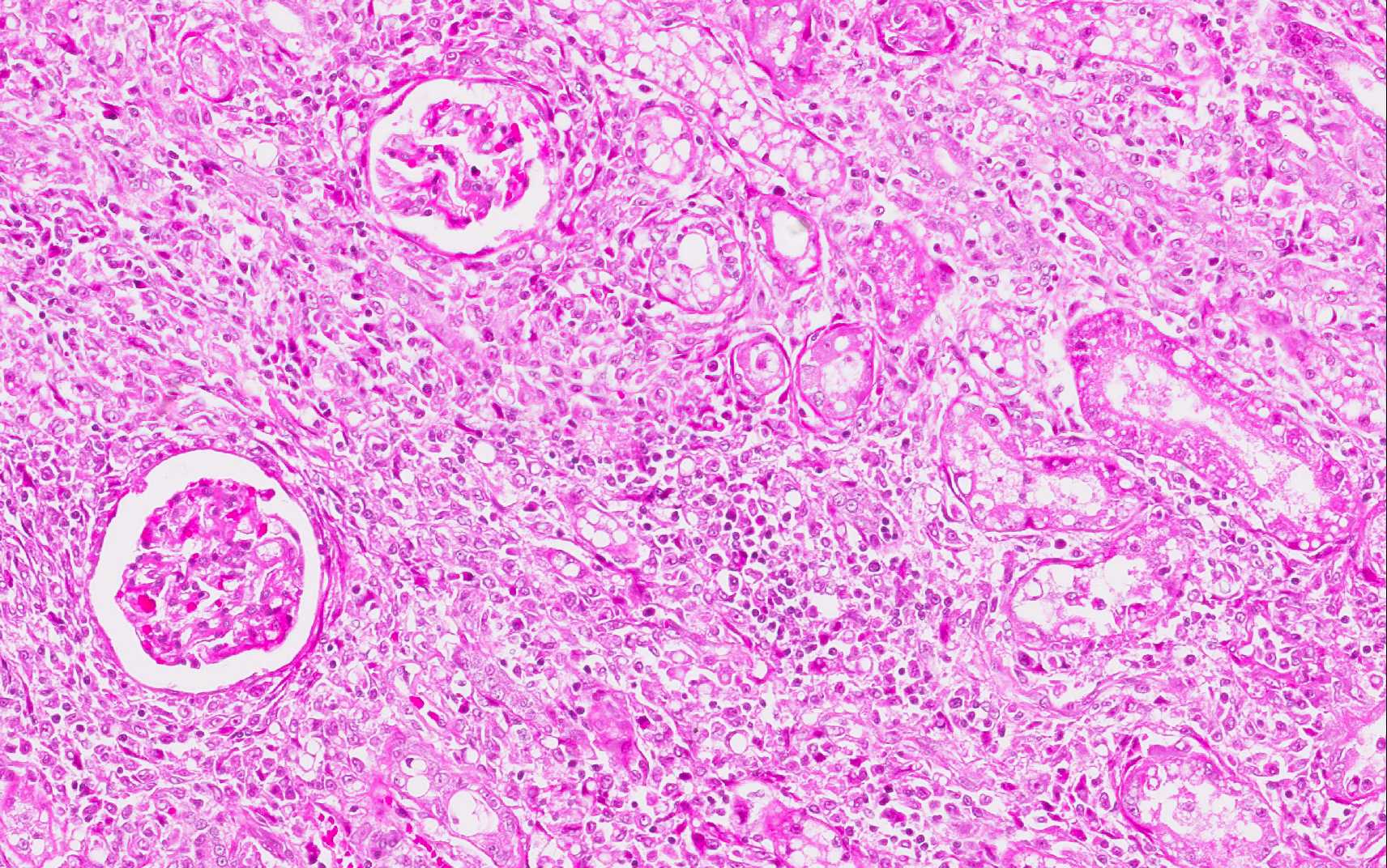
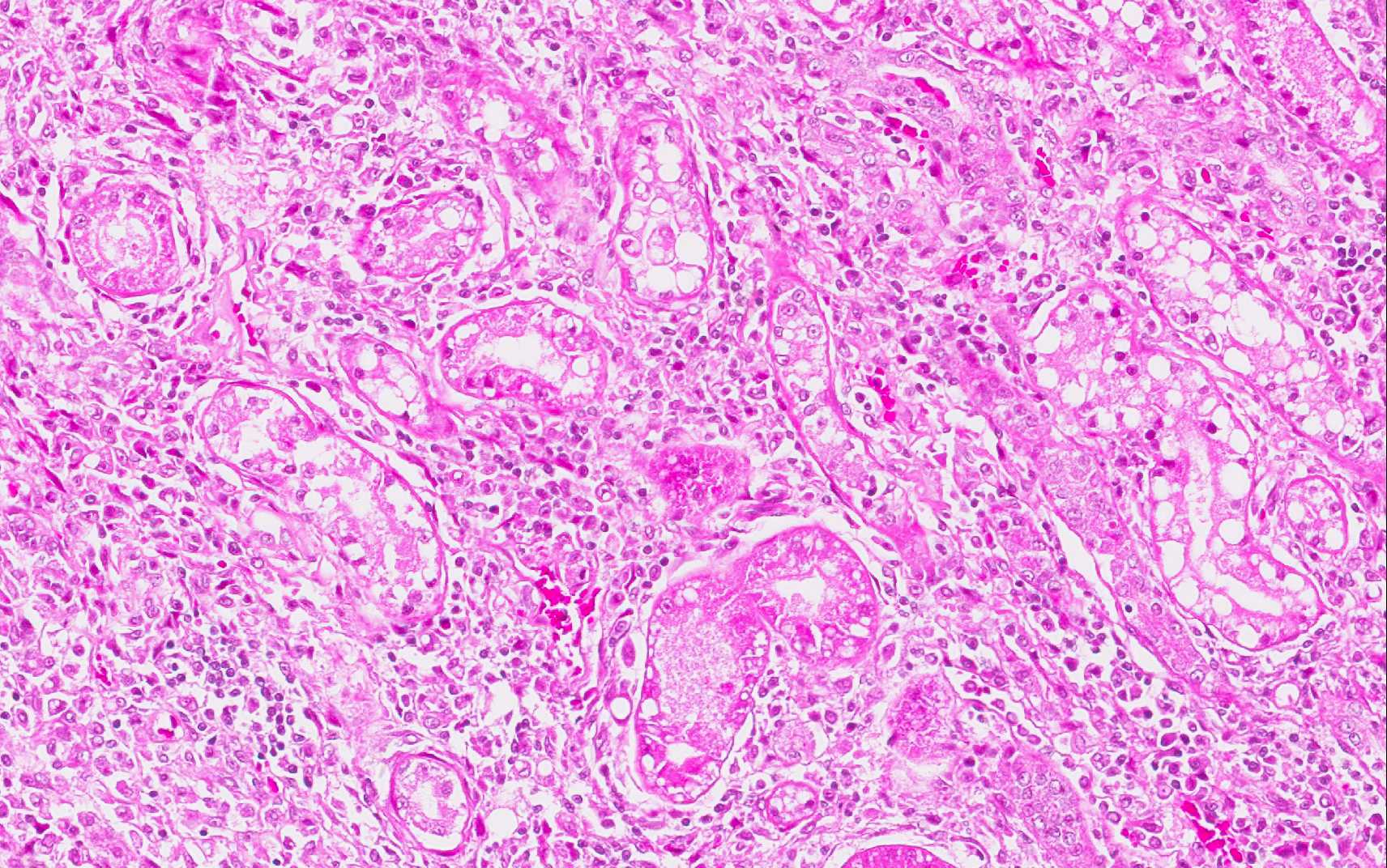
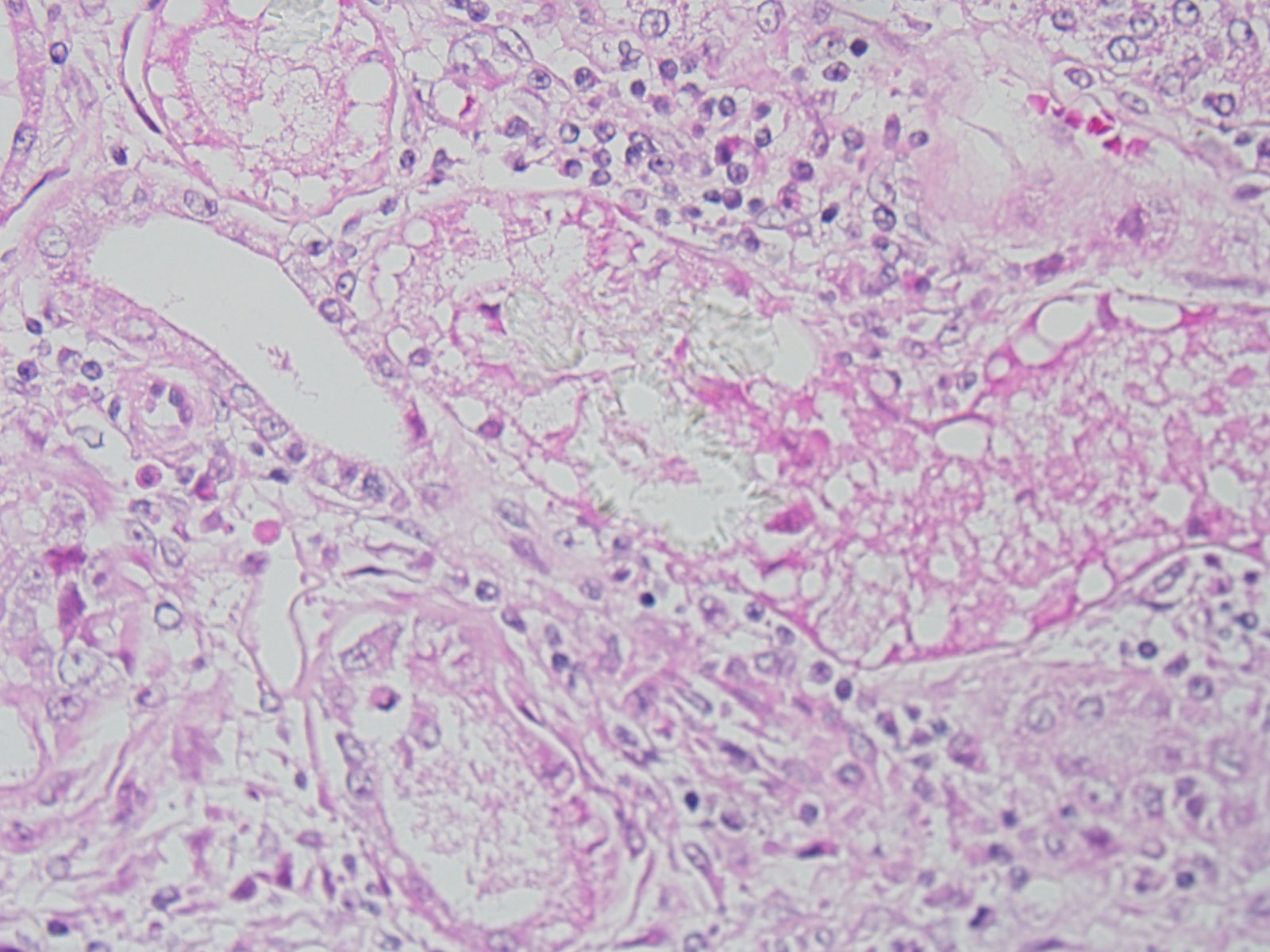
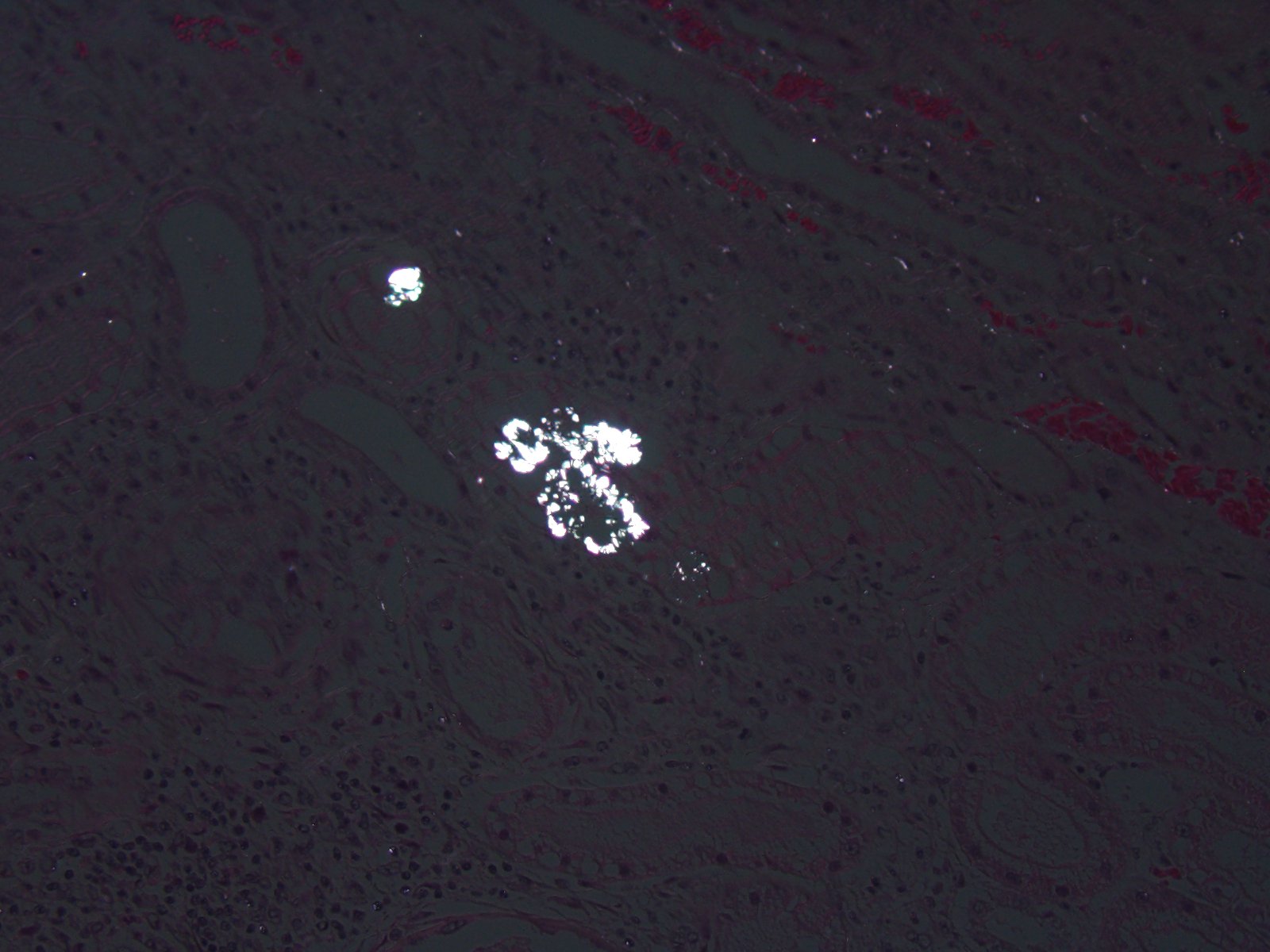
The epithelium of most tubules has undergone varying degrees of degeneration and necrosis. Cortical tubules were more severely affected than medullary tubules, and proximal convoluted tubules were more severely affected than straight tubules, thin segments, or ducts. Degenerate epithelial cells had swollen, irregularly vacuolated cytoplasm. Necrotic epithelial cells had granular eosinophilic cytoplasm and either lacked a nucleus or exhibited pyknosis and karyorrhexis. The lumens of many tubules and ducts contained eosinophilic, granular remnants of desquamated, necrotic epithelial cells, granular casts, or homogeneously eosinophilic material (hyaline casts). Lymphocytes and some macrophages had accumulated in the interstitium.
Morphologic Diagnosis:
Condition:
Contributor Comment:
The genera Lilium (Madonna lily, white lily, tiger lily, rubrum lily, Japanese show lily, devil lily, Easter lily, trumpet lily, leopard lily, panther lily, stargazer lily, Asiatic lily, wild yellow lily, and Turks cap lily) and Hemerocallis (the day lilies with flowers lasting only one day) are the groups considered potentially nephrotoxic to cats. For the purposes of our discussion, we will limit our investigation to the genera Lilium and Hemerocallis are which cause nephrotoxicity. Nevertheless, it must be kept in mind that a wide variety of plants are in the lily family or are called lilies (and hybrids exist), and within this group there is a similar diversity in the potential toxicological effects.(3)
Various members of the Lileaceae family of plants can cause acute tubular necrosis in animal species, for example, Narthedum ossifragum (bog aspodel) in ruminants, several lilies,and their hybrids (Lilium spp.)(3) Most pet owners know little about the danger these plants pose to cats. Although cats are finicky eaters, for some unknown reason they eat the leaves and flowers of Lilium plants. Both leaves and flowers are reportedly toxic. Ingestion of one or two leaves or one whole flower has caused death in cats.(3,5)
Cats are really sensitive to ingestion of certain species of lilies; no age, sex, or breed predilection has been identified.(3) The mortality rate from Easter lily toxicosis is reported to be as high as 50100%, depending on the time symptomatic treatment is initiated. High mortality rate is reported if treatment is not initiated before onset of anuric renal failure, which occurs 1824 hours after exposure.(5) Nephrotoxic damage cannot be duplicated in rats, mice, or rabbits. In dogs, only vomiting and gastrointestinal signs can be seen after lily ingestion in dogs even when fed large amounts of these plants.(3)
The exact mechanism of action of lily poisoning, specifically lily-induced nephrotoxicity, is unknown. The rapid onset of clinical signs after ingestion of culprit species indicates rapid absorption rate for the poison. The toxins damage renal tubular epithelial cells resulting in cell death and sloughing of damaged renal cells. The insult to the kidney is severe, leading initially to polyuric kidney failure. This polyuric kidney failure leads to extreme dehydration. If this dehydration progresses far enough or goes on long enough, anuric renal failure and complete renal shutdown can develop.(3)
In this case, microscopic lesions in the kidney were compatible with nephrotoxic tubular necrosis of a few days duration. Nephrotoxic tubular necrosis is not a specific diagnosis and can result from a variety of nephrotoxins, such as aminoglycoside antibiotics (e.g., gentamicin), metals (e.g., lead, arsenic, mercury), or metabolites of ethylene glycol.(2) In this case, the lily was the probable source of the nephrotoxin and the whole renal lesions.
At present, there is no gold standard test for analysis and verification of lily ingestion. The most positive confirmations involve the observation of the animal ingesting the lily, compatible clinical syndrome signs, compatible clinicopathological findings, and supportive postmortem lesions in cats that die. Even if postmortem lesions are suggestive of lily poisoning, positive verification of lily ingestion cannot be made unless ingested plant material observed within the gastrointestinal tract. Despite no specific test existing to verify this poisoning, if the index of suspicion for lily intoxication is high, initiation of appropriate fluid therapy should begin to prevent anuric renal failure from developing.(3)
JPC Diagnosis:
Conference Comment:
Seizures are also reported in addition to the renal and pancreatic changes and may occur within 8 hours after exposure.(5) The flowers of lily plants are more toxic than its leaves but ingestion of either may result in the renal changes described above. Changes within the kidney occur initially in the inner cortex, and as the condition progresses, tubules within the outer cortex succumb to damage as well. Ultrastructural changes include mitochondrial swelling in renal proximal tubule epithelium and the formation of megamitochondria, which may result from either enlargement of individual mitochondria or fusion of mitochondria. Other ultrastructural changes that have been described include pyknotic nuclei and lipid infiltration.(5)
The conference histologic description included many of the tubular features described above by the contributor. The primary findings in this case are tubule degeneration and necrosis and the inflammation is considered a secondary finding. There was discussion regarding the origin of the inflammation and whether it was a process unrelated to the tubular necrosis, and perhaps present prior to the onset of nephrotoxic tubular changes; however, a consensus opinion was not reached in this regard and thus it was included in the morphologic diagnosis with the tubular changes. Additional features include tubule regeneration and atrophy, mild glomerular changes including thickened parietal and visceral epithelium and low numbers of sloughed epithelium within the urinary space. Low numbers of birefringent crystals are also seen within tubule lumina when viewed under polarized light. The capsule is mildly expanded by hemorrhage and inflammatory cells. Although mild, the presence of glomerular lesions also lends evidence to another process taking place in the kidney as glomerular lesion are not commonly reported in cases of lily intoxication. Other nephrotoxic plants which affect domestic animal species that were discussed during the conference include Isotropis toxicity in ruminants, oak toxicity in ruminants and horses, Amaranthus retroflex us (pigweed) toxicity in swine and cattle, Lantana camera toxicity in cattle, and oxalate containing plant (i.e. Rumex spp., Oxalis cernua, Halogeton glomeratus, etc.) toxicity in cattle and sheep.(2)
References:
2. Cianciolo RE, Mohr FC. Urinary system. In: Maxie MG, ed. Jubb, Kennedy, and Palmer's Pathology of Domestic Animals. 6th ed. Vol 2. St. Louis, MO: Elsevier; 2016:421-428.
3. Fitzgerald K T. Lily Toxicity in the Cat. Top Companion Anim Med. 2010; 25(4):213-217.
4. Maxie MG, Shelley JN. Urinary system. In: Maxie MG, ed. Jubb, Kennedy and Palmers Pathology of Domestic Animals. 5th ed. Vol. 2. Philadelphia, PA: Elsevier; 2007: 472-473.
5. Rumbeiha WK, Francis JA, Fitzgerald SD, Nair MG, Holan K, Bugyei KA, Simmons H. A Comprehensive Study of Easter Lily Poisoning in Cat. J Vet Diagn Invest 2004 16: 527-541.