Signalment:
Seven-month-old, female, Golden Retriever mixed breed,
Canis familiaris, dog The dog was presented with chronic conjunctivitis, gingival lesions, and respiratory disease. The clinical signs had begun at 4.5 weeks of age and had progressed. Previous diagnostics including conjunctival biopsies, cytology and bacterial culture of conjunctival swabs, canine distemper serology, virus isolation, and routine bloodwork failed to establish a diagnosis. On presentation there were circular, raised, pink, fleshy, mucosal lesions of the conjunctiva, throughout the oral cavity and naso-pharynx and an ulcer on the soft palate. Thoracic auscultation revealed harsh referred upper airway sounds. A repeat biopsy of the ocular conjunctiva identified a profuse accumulation of fibrin in areas of ulceration and under-running the epithelium. A diagnosis of ligneous conjunctivitis was made. Based on this diagnosis and involvement of other mucosal surfaces, a presumptive diagnosis of plasminogen deficiency was made. This was confirmed by a low plasminogen functional activity assay of 35% (compared to a normal age-matched control of 111% and pooled samples from normal dogs of 118%). The conjunctival lesions recurred after the excisional biopsy. A 2-week round of topical and intravenous treatment with fresh frozen plasma diminished the conjunctival lesions; however, four weeks later the dog had a lower plasminogen activity assay (10%), weight loss, inappetance and lethargy. The owners requested euthanasia.
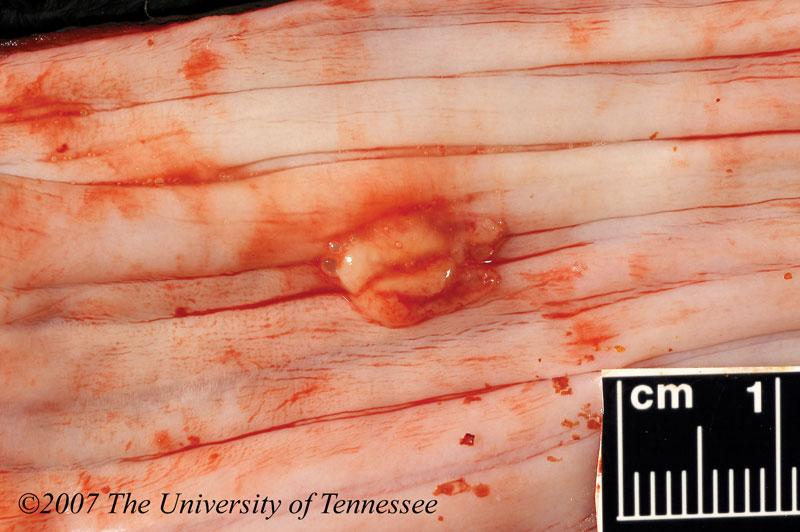
Gross Description:
Multifocal to coalescing, 0.2cm to 2.0 cm in diameter, raised, white to gray, granular, plaques decorated the glossal, buccal and gingival surfaces
(Fig 4 -1). In the soft palate, there was a 2 x 2cm ulcerated area, covered by a thick layer of a granular yellow material. There were multifocal, 0.5cm to 1cm diameter, gray plaques on the esophageal mucosa
(Fig. 4-2). Gray to yellow, granular, fibrinous plaques were disseminated over the length of the tracheal mucosa. Multifocally slightly elevated plaques covered the epicardium of the right and left ventricles. Additionally there was mild hydrocephalus, rare intestinal mucosal hemorrhages, and a mild fibrinous perihepatitis
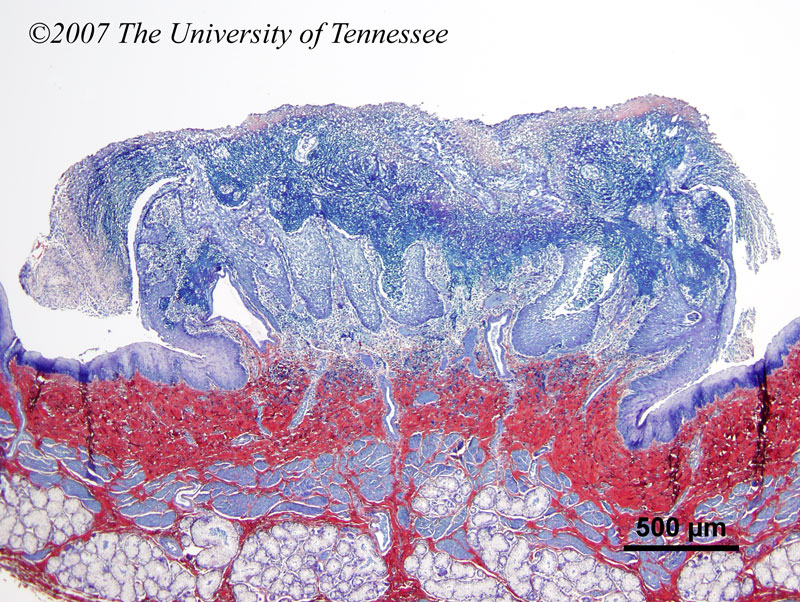
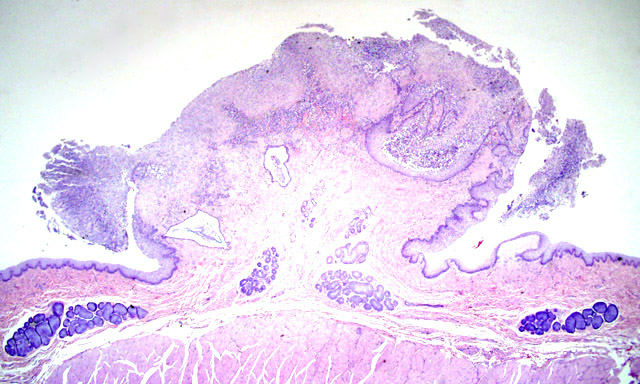
Histopathologic Description:
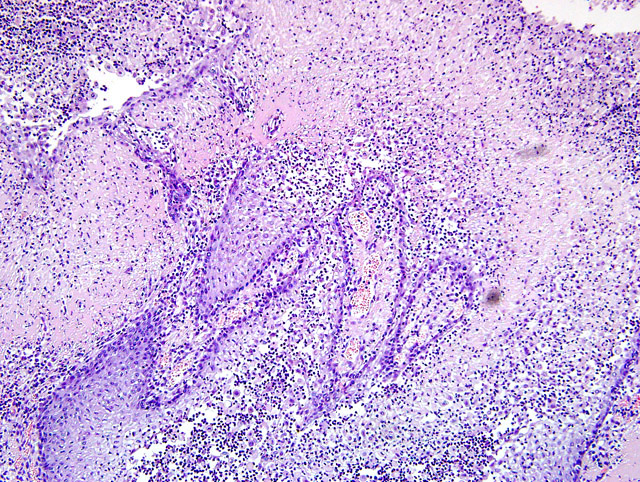
The sections of esophagus submitted have focal erosion to ulceration of locally hyperplastic epithelium covered by an exophytic coagulum of fibrin and cellular debris
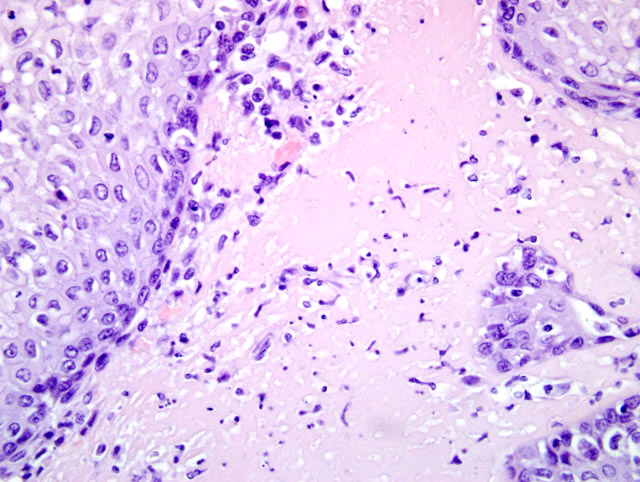
(Fig 4-3). The exophytic coagulum is supported by a pedunculated to broad base of fibrin irregularly infiltrated by granulation tissue with macrophages and neutrophils and a few lymphocytes, plasma cells and eosinophils admixed. In some areas, this thick layer of fibrin and inflammatory cells forms finger-like projections partially overlain by squamous epithelium
(Fig. 4-4). In immediately adjacent esophagus there is limited focal to multifocal subepithelial fibrin deposition
(Fig. 4-5).Â
Morphologic Diagnosis:
Severe, chronic, ulcerative and proliferative, fibrinomembranous esophagitis
Condition:
Ligneous conjunctivitis
Contributor Comment:
This patient was initially presented to the Ophthamology service because of bilateral conjunctival lesions. The clinical diagnosis of ligneous conjunctivitis was made based on the histologic appearance of the conjunctival biopsy and functional plasminogen activity assay. This form of conjunctivitis is so named because of the wood-like consistency of the membranes. Reports of this condition in canines are rare, predominantly in the Doberman Pinscher breed.
9 It is more commonly reported in females in both the veterinary and human literature.
5,9 The condition is linked to a type I plasminogen deficiency and an autosomal-recessive genetic mutation has been identified as a common cause of this functional deficiency.
10 The pathogenesis of the lesions in the conjunctiva and other mucosal sites involves the coagulation of fibrin following minor mechanical injury to tissues. This fibrin rich matrix provides hemostasis and is subsequently replaced by granulation tissue in normal individuals.Â
Impaired proteolysis due to deficiency in plasminogen results in an inability to remove the fibrin rich matrix and remodel granulation tissue, thus arresting wound healing at the granulation tissue stage and resulting in the accumulation of fibrin rich membranes.Â
The condition is typically diagnosed in neonates but may develop at any age. The palpebral conjunctiva is affected most frequently but the bulbar conjunctiva and cornea may be affected as well. Other mucosal sites such as the gingiva, ear, respiratory tract, gastrointestinal tract and female reproductive tract may also be affected with or without the presence of conjunctival lesions.
3,4,9,12 As was the case in this dog, hydrocephalus has been reported in infants with plasminogen deficiency.
4,12 In this case there were multiple venous thrombi associated with lesions in the oral cavity and present in the pulmonary field. While the primary respiratory signs in this dog were likely due to tracheal obstruction, the pulmonary thrombi may have played some role in this animals respiratory condition. Although not reported in the human literature in association with ligneous conjunctivitis, severe decreases in plasminogen activity, when coupled with other insults or precipitating events such as operations, trauma or infection have been reported to increase the risk for thromboembolic events.
8
JPC Diagnosis:
Esophagus: Esophagitis, proliferative, fibrinous, neutrophilic and lymphoplasmacytic, multifocal, marked, with ulceration, acantholysis, granulation tissue and multifocal subepithelial fibrin, Golden retriever mix (
Canis familiaris), canine.
Conference Comment:
The contributor gives an excellent overview of plasminogen deficiency associated with ligneous conjunctivitis. Conference participants are encouraged to review the article on this case published by Johnstone McLean et al.
7 Plasminogen plays a vital role in intravascular and extravascular fibrinolysis, wound healing, cell migration, tissue remodeling, angiogenesis, and embryogenesis.
2 Plasminogen may be converted to plasmin by cleavage with either tissue-type plasminogen activator (tPA) leading to lysis of fibrin clots in the blood stream or urokinase-type plasminogen activator (uPA) associated with wound healing and tissue remodeling.
1
It is interesting to note that in humans and animals diagnosed with type I plasminogen defficiency, there is little to no increase in the risk of developing intravascular thrombosis, which implies the existence of an alternative pathway for intravascular fibrinolysis.
7,11,13
The pseudomembranous deposits on mucous membranes occurs primarily in areas of previous damage. The hyaline material may contain scattered neutrophils, eosinophils, T-lymphocytes, plasma cells, mast cells and/or foreign material. Immunohistochemistry may be positive for fibrin, albumin and immunoglobulins (IgG, IgA).
3,6
References:
1. Bugge TH, Flick MJ, Danton MJ, Daugherty CC, Romer J, Dano K, Carmeliet P, Collen D, Degen JL: Urokinase-type plasminogen activator is effective in fibrin clearance in the absence of its receptor or tissue-type plasminogen activator. Proc Natl Acad Sci USA 93:5899-5904, 1996
2. Castellino FJ, Ploplis VA: Structure and function of the plasminogen/plasmin system. Thromb Haemost 93:647-654, 2005
3. Chai F, Coates H: Otolaryngeal manifestations of ligneous conjunctivitis. Int J Pediatr Otorhinolaryngol 22:760-762, 2003
4. Cifti E, Ince E, Akar N, Dogru U, Tefs K, Schuster V: Ligneous conjunctivitis, hydrocephalus, hydrocele and pulmonary involvement in a child with homozygous type I plasminogen deficiency. Eur J Pediatr 162:462-465, 2003
5. Cohen SR: Ligneous conjunctivitis: an opthalmic disease with potentially fatal tracheobronchial obstruction. Am Otol Rhinol Laryngol 99:509-512, 1990
6. Wilcock BP: Eye. In: Jubb, Kennedy, and Palmers Pathology of Domestic Animals, ed. Maxie MG, 5th ed., vol. 1, p. 481. Elsevier Limited, St. Louis, MO, 2007
7. Johnstone McLean NS, Ward DA, Hendrix DV, Donnell RL, Ilha MR: Ligneous conjunctivitis secondary to a congenital plasminogen deficiency in a dog. J Am Vet Med Assoc 232:715-721, 2008
8. Lottenberg R, Dolly JR, Kitchens CS: Recurrent thromboembolic disease and pulmonary hypertension associated with severe hypoplasminogenia. Am J Hematol 168:181-193, 1985
9. Ramsey DT, Ketring KL, Glaze MB, Knight B, Render JA: Ligneous conjunctivitis in four doberman pinschers. J Am Anim Hosp Assoc 32:439-447, 1996
10. Schuster V, Zeitler P, Seregard S, Ozcelik U, Anadol D, Lutchman-Jones L, Meire F, Mingers AM, chambeck C, Kreth HW: Homozygous and compoundheterozygous type I plasminogen deficiency is a common cause of ligneous conjunctivitis. Thromb Haemost 85:1004-1010, 2001
11. Schuster V, Hugle B, Tefs K: Plasminogen deficiency. J Thromb Haemost 5:2315-2322, 2007
12. Scully C, Allen C, Ervesen G, Hodgson T, Speight P: Oral lesions indicative of plasminogen deficiency (hypoplasminogenemia). Oral Surg Oral Med Oral Pathol Radiol Endod 91:334-337, 2001
13. Shigekiyo T, Uno Y, Tomonari A, Satoh K, Hondo H, Udea S, Saito S: Type I congenital plasminogen deficiency is not a risk factor for thrombosis. Thromb Haemost 67:189-192, 1992