Signalment:
Gross Description:
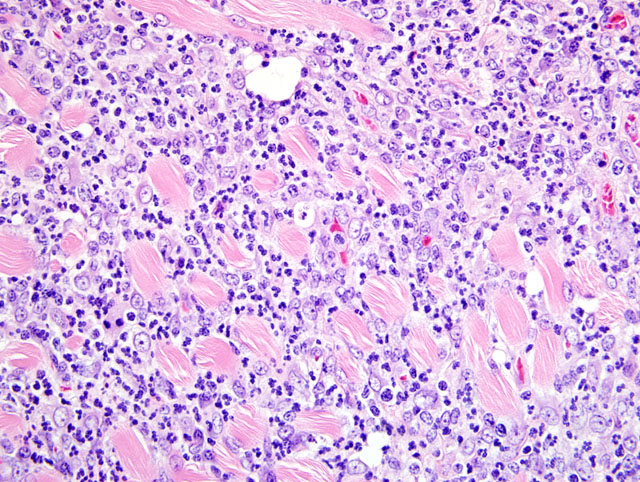
Histopathologic Description:
Morphologic Diagnosis:
Lab Results:
| Hematology | Reference Ranges* | WBC Diff. (%) (x10E9/L) | Reference Ranges* (%) |
| WBC 19.7 x10E9/L | 7.7 15.4 x10E9/L | Segs 49% 9.653 | 24 78% |
| RBC 6.33 x10E12/L | 7.3 12.18 x10E12/L | Bands 1% 0.197 | 0 2.2% |
| HGB 98 g/L | 120 182 g/L | Eos 7% 1.379 | 0 7% |
| HCT 0.266 L/L | 0.36 0.61 L/L | Lymph 40% 7.880 | 28 69% |
| Mono 3% 0.591 | 3.4 8.2% | ||
| Platelets: Clumped | |||
| Corr. WBC 19.7 x10E9/L | |||
| RBC Morphology | Anisocytosis 1+ |
| Biochemistry Results | Reference ranges* | Biochemistry Results | Reference ranges* |
| Sodium 145 mmol/L | 146 160 | Amylase 9 U/L | |
| Potassium 5.4 mmol/L | 4.3 5.3 | Alk.Phos. 9 U/L | 30 120 |
| Na:K Ratio 27 | CK 110 U/L | ||
| Chloride 117 mmol/L | 102 121 | AST [GOT] 63 U/L | |
| Calcium 2.12 mmol/L | 2.15 2.62 | ALT [GPT] 67 U/L | 82 289 |
| Phosph. 1.83 mmol/L | 1.81 2.81 | Gamma-GT 0 U/L | |
| Urea 4.8 mmol/L | 4.28 15.35 | T. Prot. 53 g/L | |
| Creat. 16 umol/L | 17 53 | Albumin 21 g/L | |
| Glucose 7.3 mmol/L | 3.47 7.44 | Globulin 32 g/L | |
| Cholest. 4.29 mmol/L | 1.65 7.64 | A:G Ratio: 0.66 | |
| T. Bili. 1 umol/L | <17 | Lipase 278 U/L |
Condition:
Contributor Comment:
Myofasciitis in domestic ferrets is an idiopathic disease characterized by suppurative to pyogranulomatous myositis and fasciitis affecting skeletal, smooth, and cardiac muscle and associated fascial connective tissues.(4) As the condition is disseminated and muscle is the predominant target tissue, the terms polymyositis and disseminated idiopathic myositis have also been used in this condition. But, as the inflammation extends into the fascia and adipose tissue around muscle bundles, myofasciitis was thought to be a more appropriate morphologic descriptor for this condition.(4)
The disease affects young adults of both sexes and is clinically characterized by rapid onset of clinical signs: weakness, muscle atrophy or lethargy, high fever, neutrophilic leukocytosis, treatment failure and death (or euthanasia). The primary presenting sign may be an ambulatory problem, primarily recognized clinically in the hindlimbs.(4) Inflammation of the alimentary smooth muscle may result in clinical presentation due to various alimentary tract problems.(4) Gross lesions seen at the time of necropsy often include atrophy of skeletal muscle, red and white mottling and dilation of the esophagus, and splenomegaly. Upon histologic examination, suppurative to pyogranulomatous inflammation in the skeletal muscle and fascia of limbs, lumbar region, body wall, head, heart, and/or esophagus is seen. The extensive suppurative to pyogranulomatous esophagitis which can be diffuse and circumferential is thought to be a unique feature of this disease. Splenic enlargement is due to myeloid hyperplasia, which can also be seen in the bone marrow.(4) In this case, suppurative to pyogranulomatous esophagitis, suppurative to pyogranulomatous hind limb myositis, suppurative to pyogranulomatous periarteritis/pericarditis and splenic myeloid hyperplasia were observed.
On CBC, a neutrophilic leukocytosis, as seen in this case, may be observed.(4) Upon evaluation of serum chemistries, no elevations of creatine kinase (CK) or aspartate aminotransferase (AST), indicators of muscle damage, have been associated with the disease and elevations of these enzyme activities were not seen in this case. This may be because the inflammation displaces and results in atrophy of the muscles rather than resulting in significant myodegeneration or myonecrosis.(4) Alanine aminotransferase (ALT) may be mildly elevated in some cases, possibly due to muscular or hepatic damage, but such an elevation was not noted in this case.
The pathogenesis of ferret myofasciitis is unclear; possibilities considered include infectious or vaccine-related mechanisms of immune mediated disease. In a recent review paper, Garner et al. (2007) investigated some possible infectious etiologies including histologic and electron microscopic evaluation for viral inclusion bodies and viral particles, immunohistochemical staining for feline and ferret coronaviral antigens, and histologic examination and immunohistochemical staining for protozoal antigens (for Toxoplasma gondii, Neospora caninum, and Sarcocystis neurona); the studies did not reveal any intralesional infectious agents.4 However, these negative findings do not rule out the possibility of an infectious process being involved in the etiopathogenesis of this disease.
In childhood idiopathic inflammatory myopathies it has been proposed that environmental triggers in the setting of an underlying genetic susceptibility may play a role in the etiopathogenesis of the lesions.(3) With regards to genetic susceptibility, specific HLA alleles have been found to be immunogenic risk factors for juvenile dermatomyositis in humans. In dogs, the association of distinct inflammatory myopathies with certain dog breeds suggests that genetic predispositions are involved in the development of canine inflammatory myopathies.(7) Garner et al. (2007) thought that a heritable basis for myofasciitis seemed unlikely as affected ferrets are from different breeding facilities and the disease has been seen in both the USA and The Netherlands.
An adverse vaccine reaction is also a consideration as a possible cause in this disease. All of the ferrets affected have been reported to have had a least one dose of canine distemper vaccine.(4) In humans, macrophagic myositis is a recently described condition in adults and (less frequently) children which develops focally after injection of aluminum-containing vaccines.(5,6) The conspicuous macrophages within the inflammatory lesion have intensely PAS-positive cytoplasm due to intralysosomal accumulation of aluminum hydroxide, an adjuvant used in vaccines. Difficulty in clearing aluminum from the injection site and abnormal immune response to prolonged tissue retention of aluminum hydroxide is considered to be the etiology of the lesion.(6) No evidence of similar lysosomal accumulation of aluminum hydroxide was observed upon electron microscopic evaluation of domestic ferrets with myofasciitis. If a vaccine is involved, a delayed-type immune reaction to a vaccinal substance (killed or modified infectious agent, adjuvant, residual substance, or contaminant) may be involved.(4)
In conclusion, myofasciitis in domestic ferrets is an idiopathic disease characterized by suppurative to pyogranulomatous myositis and fasciitis affecting skeletal, smooth, and cardiac muscle and associated fascia. The circumferential suppurative to pyogranulomatous esophagitis appears to be unique to this condition. The disease is unresponsive to medical treatments and appears to be uniformly fatal.
JPC Diagnosis:
Conference Comment:
References:
2. Evans J, Levesque D, Shelton GD: Canine inflammatory myopathies: a clinicopathologic review of 200 cases. J Vet Intern Med 18:679-91, 2004
3. Feldman BM, Rider LG, Reed AM, Pachman LM: Juvenile dermatomyositis and other idiopathic inflammatory myopathies of childhood. Lancet 371:2201-12, 2008
4. Garner MM, Ramsell K, Schoemaker NJ, Sidor IF, Nordhausen RW, Bolin S, Evermann JF, Kiupel M: Myofasciitis in the domestic ferret. Vet Pathol 44:25-38, 2007
5. Hewer E, Goebel HH: Myopathology of non-infectious inflammatory myopathies - the current status. Pathol Res Pract 204:609-23, 2008
6. Lach B, Cupler EJ: Macrophagic myositis in children is a localized reaction to vaccination. J Child Neurol 23:614-9, 2008
7. Shelton GD: From dog to man: the broad spectrum of inflammatory myopathies. Neuromuscul Disord 17:663-70, 2007