CASE III: 18-33 (JPC 4135937)
Signalment:
8 week old female Ragdoll kitten (Felis catus)
History:
The kitten was shut in a closet overnight, and in the morning was found by the owner curled up on the floor in the closet with red-brown, gelatinous material oozing from her mouth. The owner identified a live wire protruding from the floor that shocked her when touched. The kitten was subsequently presented to an emergency veterinarian for further evaluation. On physical examination the cat was markedly painful around the mouth, dull, and weak. Numerous extensive burn wounds were identified on the lips, tongue, and palate. Given the extent of the lesions and poor prognosis for healing of wounds in the oral cavity, the kitten was euthanized.
Gross Pathology:
There was moderate, regional swelling within the soft tissues surrounding the mandible and ventral neck. Multifocally at the oral commissures, along the mandibular and maxillary gingiva, on the rostral 1/3 of the tongue, and the rostral half of the hard palate to the level of the maxillary incisors, were variably sized (2 ? 20 mm diameter) full thickness ulcerations covered by brown to gray to black, friable and sloughing tissue. Multifocally, tissue surrounding ulcers was discolored pale tan to gray. Additionally, on internal examination there was regional dark red discoloration of caudodorsal lung fields.
Laboratory Results:
Upon admission to the veterinary hospital, a complete blood count (CBC) and serum biochemistry panel were performed. CBC revealed a mild neutrophilia (interpreted as a stress leukogram) and moderate thrombocytosis. Significant serum biochemistry panel findings included a markedly elevated creatinine kinase (10,397 IU/L; RR 60 ? 531 IU/L), mildly elevated AST (166 IU/L; RR 11 ? 40 IU/L), and a mild hyperkalemia (5.7 mmol/L; RR 3.5-5.1 mmol/L). All of these findings were considered attributable to regional skeletal muscle damage from electrothermal injury.
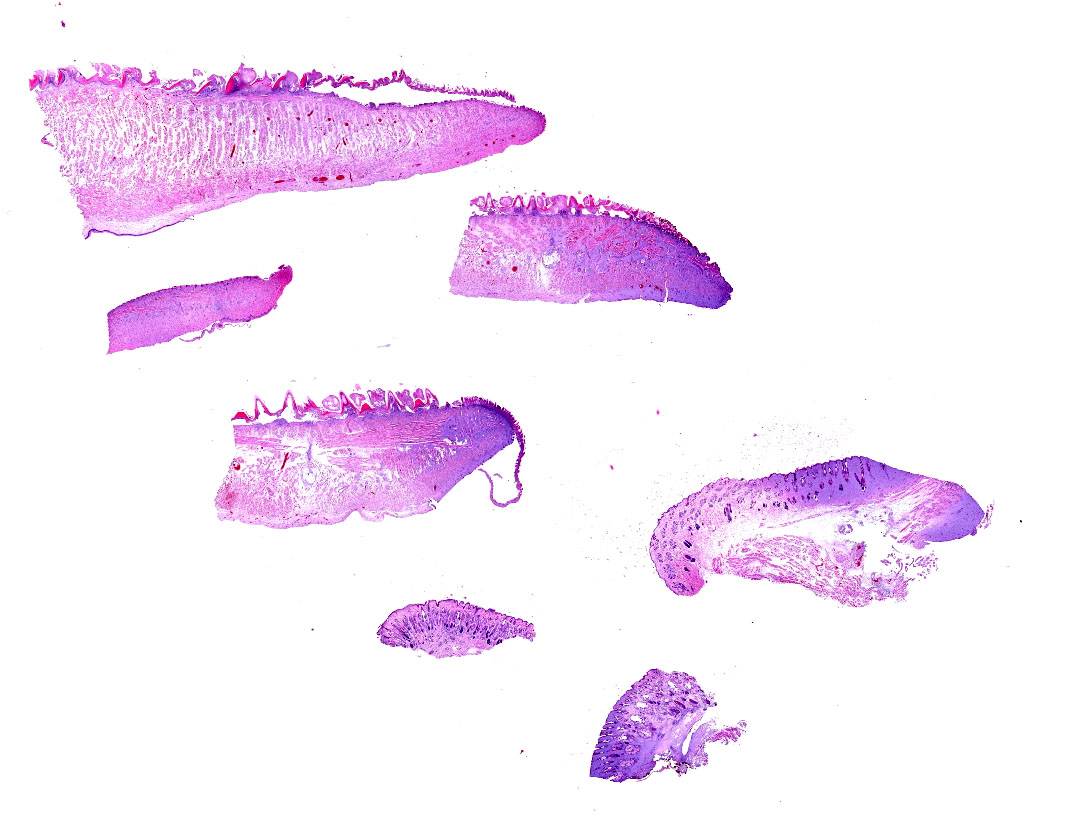
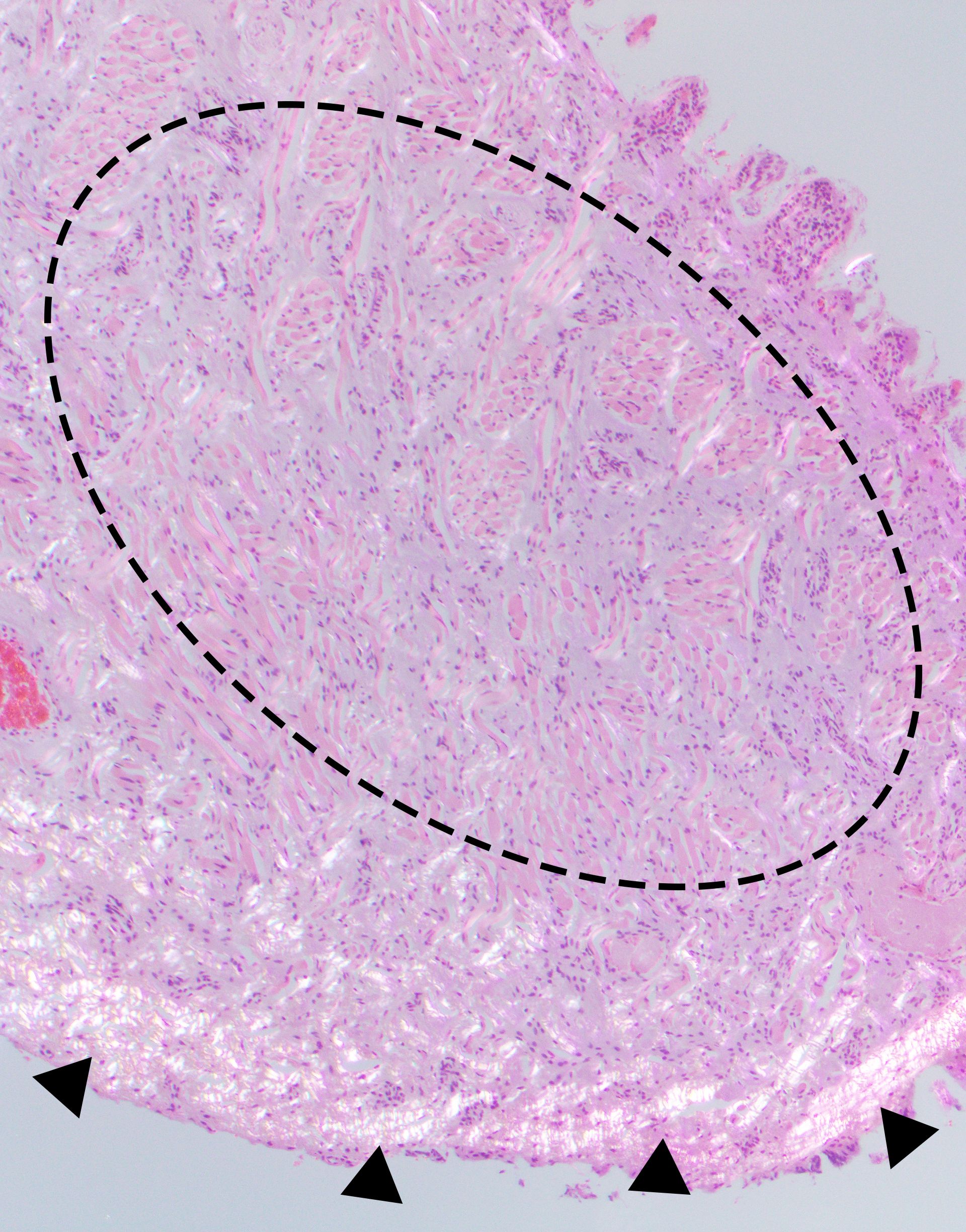
Microscopic Description:
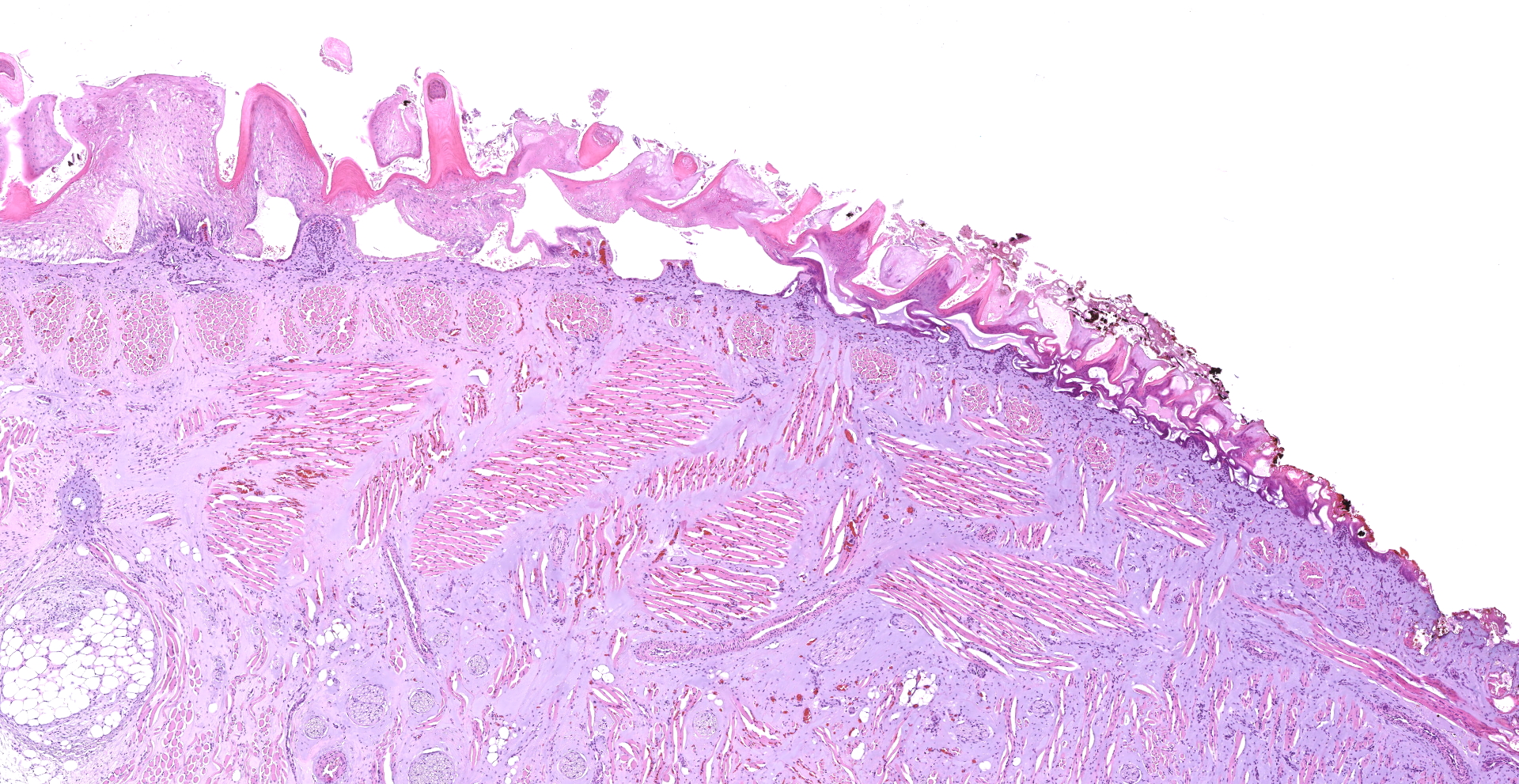
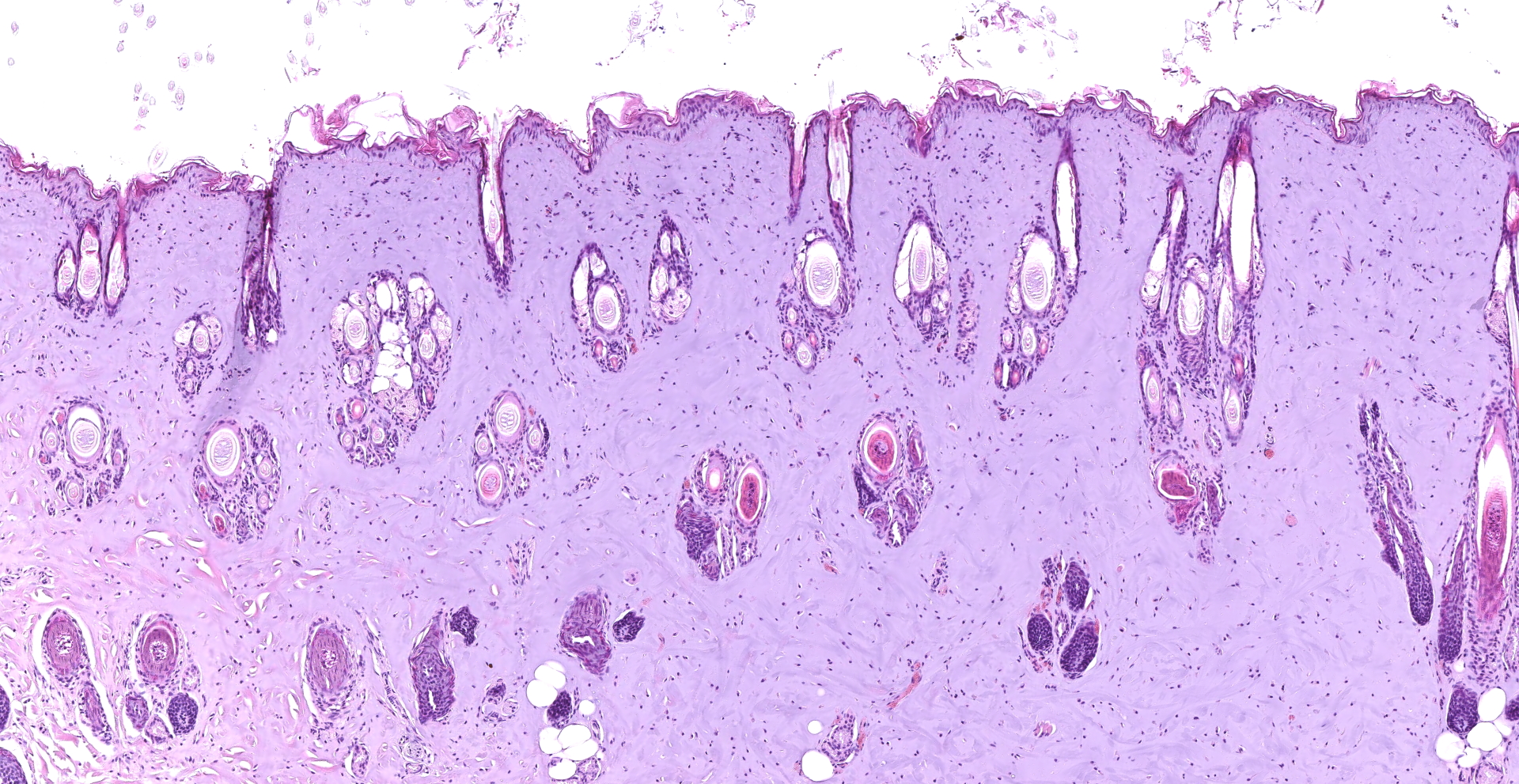
Tongue and Lips: Four sections of tongue and three sections of lip skin are examined and have similar histologic features that are described together. Multifocally, there is variable intraepidermal/mucosal and/or subepidermal/mucosal clefting, resulting in multifocal vesicle formation, erosion, and regionally extensive detachment of the epithelium/mucosa (ulceration). There is multifocal to coalescing nuclear elongation/streaming of basal cells in a ?fish bone? type pattern, and affected nuclei are hyperchromatic to pyknotic. At the areas of ulceration and vesicle formation, there are multifocal aggregates of mixed bacterial organisms (rods and cocci), mild multifocal hemorrhage, and occasional aggregates of black granular material (presumptive metallization). In the rostral third to half of examined sections of tongue, and variably identified in examined skin sections, there is loss of distinction of dermal/submucosal collagen fibers, which gradually merge into an amphophilic, amorphous coagulum (collagen homogenization). When viewed with polarized light, this collagen lacks normal birefringence. Multifocally within the dermis and submucosa, the walls of vessels are smudged with nuclear pyknosis and streaming. Multifocally, skeletal muscle fibers exhibit sarcoplasmic hypereosinophilia and vacuolation, loss of cross striations, and nuclear pyknosis. In some sections, there is mild to moderate, multifocal edema with scattered intermixed hemorrhage within the submucosa and between individual myofibers.
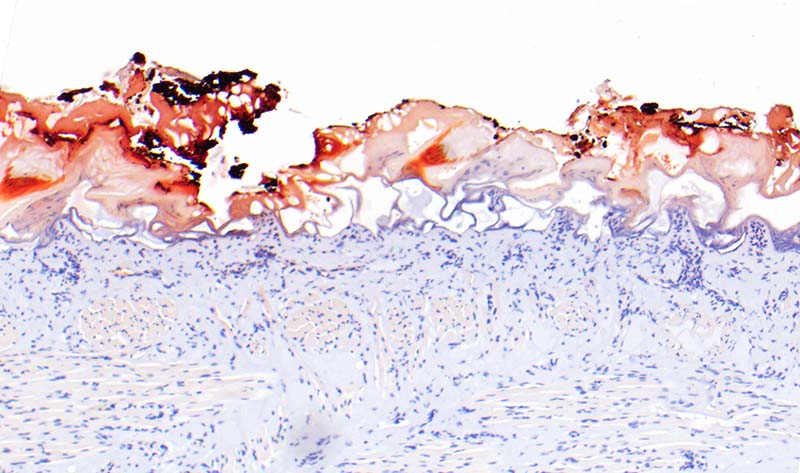
Perl's Prussian blue and rhodanine histochemical stains are applied to tissues. Multifocally, black granular material and adjacent necrotic tissue exhibits strong positive staining for copper.
Contributor's Morphologic Diagnoses:
Lips and tongue: Marked, regionally extensive, coagulative necrosis with subepidermal and intraepidermal clefting, multifocal ulceration, epidermal nuclear streaming, collagen homogenization, and metallization (consistent with electrothermal injury)
Contributor's Comment:
This is a case of clinically confirmed electrocution for which multiple classic histologic features are present.
In veterinary patients, electrical injuries most commonly occur as accidents or, in the case of outdoor grazing animals, lightning strike.4 Accidental electrical injuries can be further delineated into either low or high voltage exposure. In this case, accidental electrocution occurred from chewing on a live electrical wire connected to a household circuit, which is most consistent with a low voltage exposure. In general, high voltage exposure should theoretically have a higher propensity for more extensive injury. However, as seen in this case, low voltage accidents can result in profound external injury (electrothermal burn) with prolonged contact 4, a small contact surface area, and with a media (saliva) to further promote electrical conduction.
Characteristic microscopic features of electrothermal burns resulting from electrocution include changes to both the epidermis and dermal collagen as well as deposition of metal within affected tissue, all of which are present in this case.
First, within the epidermis, there is formation of both intra- and subepidermal vesicles, which form a ?honeycomb pattern? when numerous vesicles are present adjacent to one another.4 Furthermore, there is profound elongation of epidermal cells, with tight packing of pyknotic, elongated nuclei, also termed a ?fishbone-like? elongation.4 This feature was previously thought to be due to polarization of cells from the passing of electrical current, but has since been instead postulated to be secondary to heat injury, as the same morphologic feature can be seen in flame injury burns.2
Second, within the dermis, collagen fibers lose distinction and instead can form a large coagulum, known as ?collagen homogenization?.2,3 Affected collagen stains basophilic, and has loss of birefringence when viewed under polarized light. Depending on the extent of injury, this homogenization can extend and affect collagenous stroma in various deeper tissues, such as those surrounding vessels and nerves in this case.
Third, microscopic beads of metal can be transferred from conductive metals to the affected tissue, a phenomenon known as ?metallization.4? This finding is not specific for electrocution, as it can also be seen in thermal injury from fires. However, metallization in cases of electrocution has been noted more likely to be concentrated at the margins of wounds, or penetrate deeper into tissues. In contrast, in cases of flame injury metal tends to be more diffusely but superficially distributed.4 Histochemical stains for iron and copper can aid in identification of metal within tissues. In this case, black granular pigment was present in the epidermis of the tongue along margins of necrosis and in severely affected areas. Perl's Prussian blue and rhodanine histochemical stains were applied to tissues, and granular material exhibited strong positive staining with rhodanine stain, confirming the presence of copper metallization. Additional small positive staining beads were also present throughout the necrotic epithelium.
From a forensic perspective, when investigating the nature of external lesions in which electrocution is suspected, it can be challenging to both grossly and histologically differentiate lesions caused by electrocution, flame, or impact (abrasions).2 While the previously described microscopic features are most commonly seen in cases of electrocution, these features can also variably be seen in either flame injury or impact abrasions.2 In a study comparing histologic changes from these injuries in humans, tight packing of pyknotic nuclei was the most specific feature distinguishing electrocution injury from flame injury or impact abrasions.2 Given the overlap in histologic features that can be seen in these injuries, extensive investigation into clinical history, if possible, is helpful in case work up. In this case, the clinical history of this patient confirms that identified lesions can be attributed to electrocution.
In addition to tissues on the submitted slide, similar lesions were also present on examined sections of hard palate and adjacent nasal turbinates, with rare evidence of Wallerian-type degeneration in peripheral nerve fibers captured in section.
In addition to external injuries incurred from electrical injury, internal injuries are also possible, and organs affected depend on the flow of current through the body, with endothelial cells, muscle (skeletal and cardiac), and central nervous system most often being affected. Internal injury is rare in cases of low-voltage electrocution, and in this case, there was no evidence either clinically or on postmortem examination of injury to the heart or central nervous system. However, this patient did have gross and histologic evidence of non-cardiogenic (caudodorsally distributed) pulmonary edema, which can be seen in cases of low voltage electrical injury.5,6 The pathophysiology of electrocution-induced pulmonary edema is not completely understood, but is thought to be caused by either direct endothelial damage from electricity, or represent a form of neurogenic pulmonary edema, in which catecholamine release results in pulmonary hypertension and increased vascular permeability.1
Contributing Institution:
North Carolina State University, College of Veterinary Medicine, Department of Population Health and Pathobiology
https://cvm.ncsu.edu/research/departments/dphp/programs/pathology
JPC Diagnosis:
Oral mucosa and haired skin: Epithelial necrosis, coagulative, focally extensive, with subepithelial clefting, ulceration, nuclear streaming of the stratum basale, and subepithelial collagen homogenization and edema.
JPC Comment:
The contributor provides an excellent review of histologic lesions associated with electrothermal injury, a potentially challenging diagnosis to determine in cases lacking sufficient history and context.
There are multiple classifications of in regard the voltages associated with the power grid, including high, moderate, and low. High voltage transmission lines are typically equal to or greater than 60 kilovolts (kV). Moderate voltages are typically associated with local distribution lines, which carry electricity from distribution stations to residences and businesses; their voltage typically ranges from 2.4-60kV. Transformers lower the distribution line voltage to 600V or less (i.e. low voltage) prior to the current entering individual service lines connected to homes. For simplification, some publications discussing electrocution associate the term "low-voltage" with less than 600V whereas those with greater than 600V are ?high voltage?.3
Electrocution occurs when an animal makes contact with two pieces of electrical equipment (e.g. power lines) or is in contact with both electricity and a grounded object. Once the circuit is established, the electricity's path determines which tissues are affected, which are typically those occupying the shortest distance between the entry and exit points in high-voltage situations. The most likely cause of death in high-voltage situations is the result of current passing through the cardiac and/or respiratory centers of the CNS or directly through the heart, resulting in cardiac and/or pulmonary arrest. Notably, ventricular fibrillation precedes cardiac arrest in low voltage electrocutions but does not occur in high voltage electrocutions.3
Two forms of electrothrermal injury occur at the cellular level, with the type of injury dependent on the cell's size as well as its resistance to electrical current. The passage of electrical current through tissues generates heat, which in turn results in the formation of pores in cell membranes in a process known as electroporation. Electroporation typically affects larger cells, such as neurons and myocytes, while also correlating with the current's path. In contrast, thermal injury is more likely to occur in regions of higher resistance, such as the epidermis and dermis in this case.3
Electrocution is a significant problem in large birds, such as raptors. A review evaluating necropsy methods and findings associated with power line electrocution in raptors found 18% had a single external burn measuring less than 3cm. In cases where electrocution injury is not clear, the author recommends close evaluation of the undersides of wings distal to the elbow and lower legs and feet, which were the most common location for small isolated burns. In addition, charred tissues (e.g. skin, feathers, and beak keratin) exposed to an alternate light source at 530-570 nm under a red filter will photoluminesce bright red; unaffected or dirty tissues will photoluminesce poorly or not at all. Electrocution should always be considered as a differential for dead birds found under power lines; however, a thorough necropsy is required for this diagnosis as other possible causes of death in these areas include collisions and gunshot. The majority of avian electrocutions are reported to occur in association with distribution lines.3
A historical review of the early study of the pathophysiology associated with electrocution, as well as electricity's paradoxical ability to save lives, provides for an interesting detour.
Commercially available electricity became increasingly popular following the invention practical generators during the 1870s, which was inherently associated with many accidental deaths, particularly amongst utility workers. Early hypotheses in regard to the pathogenesis of electrocution included theories such as arterial blood's loss of magnetic properties. Medical interest was so great at the time that 12 physicians attended the execution of William Kemmler, the first legal execution by electrocution, on August 6th 1890. Although an extensive autopsy was performed, the underlying cause of death remained largely unknown.1
In 1899, Italian physiologists Jean Louis Prevost and Frederic Battelli as well as Columbia University's RH Cunningham independently demonstrated strong electrical current stopped the hearts of experimental animals while weaker shocks caused ventricular fibrillation, also resulting in death. In addition, Prevost and Battelli noted some cases demonstrating ventricular fibrillation were restored to a normal sinus rhythm after a second shock was applied to electrodes in the mouth and the intestine, unknowingly performing the first successful internal defibrillation. The significance of the event went largely unnoticed at the time since ventricular fibrillation was thought to only occur in animals and the phenomenon could not be consistently replicated nor explained.1
The invention of the electrocardiograph greatly facilitated the understanding of cardiac electrophysiology, with the first account of a recorded electrocardiograph attributed to Augustus Desire Waller in 1887. It was developed into a clinical tool over the following decades, greatly enhancing the understanding of arrhythmias and cardiac physiology. Notably, researchers identified a refractory period in the cardiac cycle during which the ventricles were more susceptible to ventricular fibrillation as the result of an electrical shock. Carl Wiggers and Rene Wegria conclusively demonstrated this in 1940, finding that a brief electrical shock only 'induces fibrillation when the shocks fall during the vulnerable period of late systole'.1
The first successful human defibrillation was performed by Claude Beck in 1947 on a 14-year old boy suffering ventricular fibrillation during an operation for pectus excavatum during which the thorax was already open. The paddles were applied directly to the heart and four shocks of 110V were delivered, saving the boy's life.1
References:
1. Ball CM, Featherstone PJ. Early history of defibrillation. Anaesth Intensive Care. 2019;47(2):112-115.
2. Caswell JL and Williams KJ. Respiratory System. In: Maxie MG, ed. Jubb, Kennedy, and Palmer's Pathology of Domestic Animals. Vol 2. 6th Ed. St. Louis, Elsevier; 2016: 487-489.
3. Kagan RA. Electrocution of Raptors on Power Lines: A Review of Necropsy Methods and Findings. Vet Pathol. 2016;53(5):1030-1036.
4. Sangita C, Garima G, Jayanthi Y, Arneet A, Neelkamal K. Histological indicators of cutaneous lesions caused by electrocution, flame burn and impact abrasion. Med Sci Law. 2018;58(4):216-221.
5. Schulze C, Peters M, Baumgärtner W, Wohlsein P. Electrical Injuries in Animals: Causes, Pathogenesis, and Morphological Findings. Vet Pathol. 2016;53(5):1018-1029.
6. Singh S, Sankar J, Dubey N. Non-cardiogenic pulmonary oedema following accidental electrocution in a toddler. BMJ Case Rep. 2011;2011:bcr0120113749. Published 2011 Apr
7. Truong T, Le TV, Smith DL, Kantrow SP, Tran VN. Low-voltage electricity-induced lung injury. Respirol Case Rep. 2017;6(2):e00292. Published 2017 Dec 22.