Signalment:
Gross Description:
Histopathologic Description:
Morphologic Diagnosis:
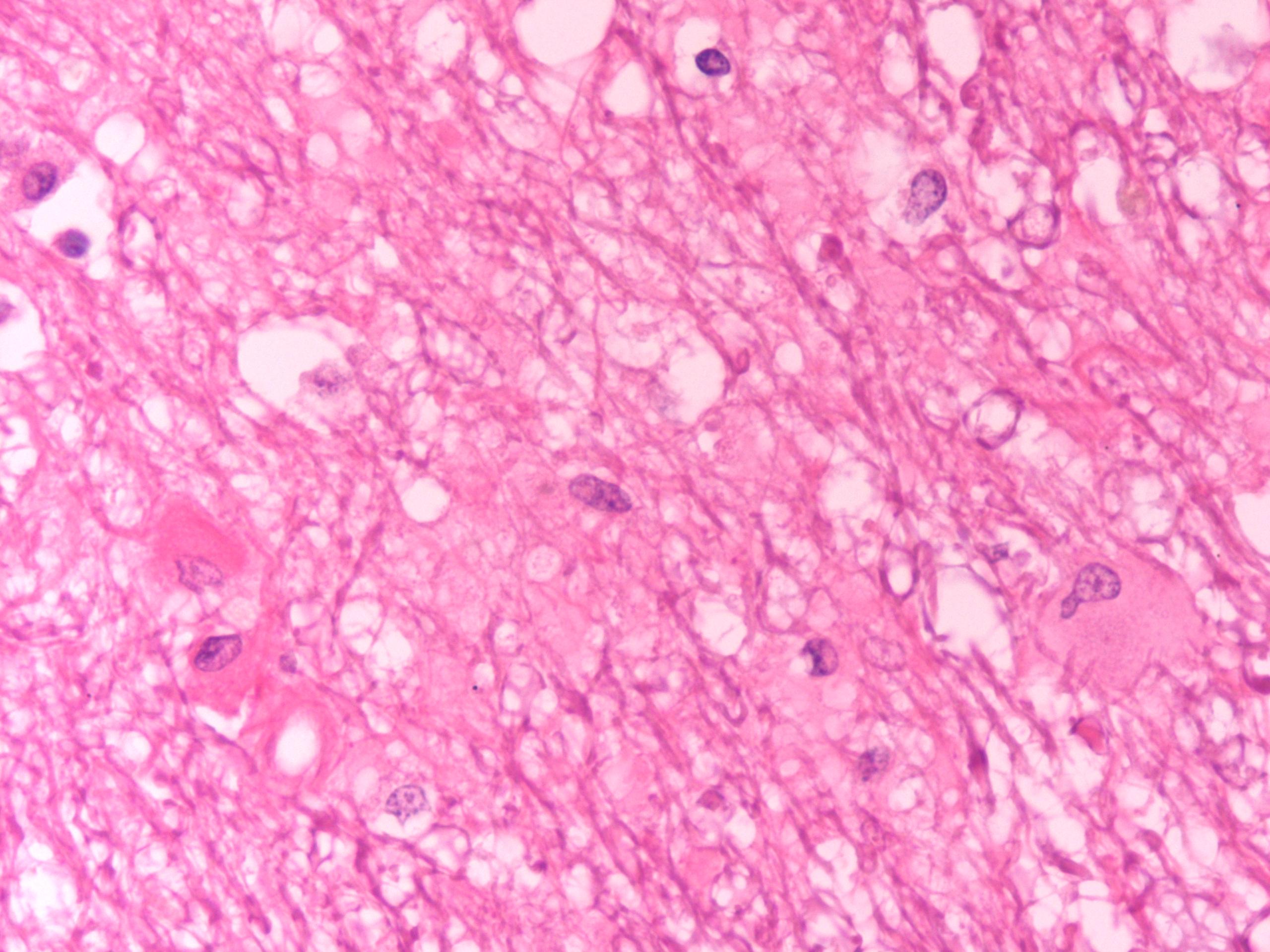
1. Edema, diffuse, severe, cerebral white matter.
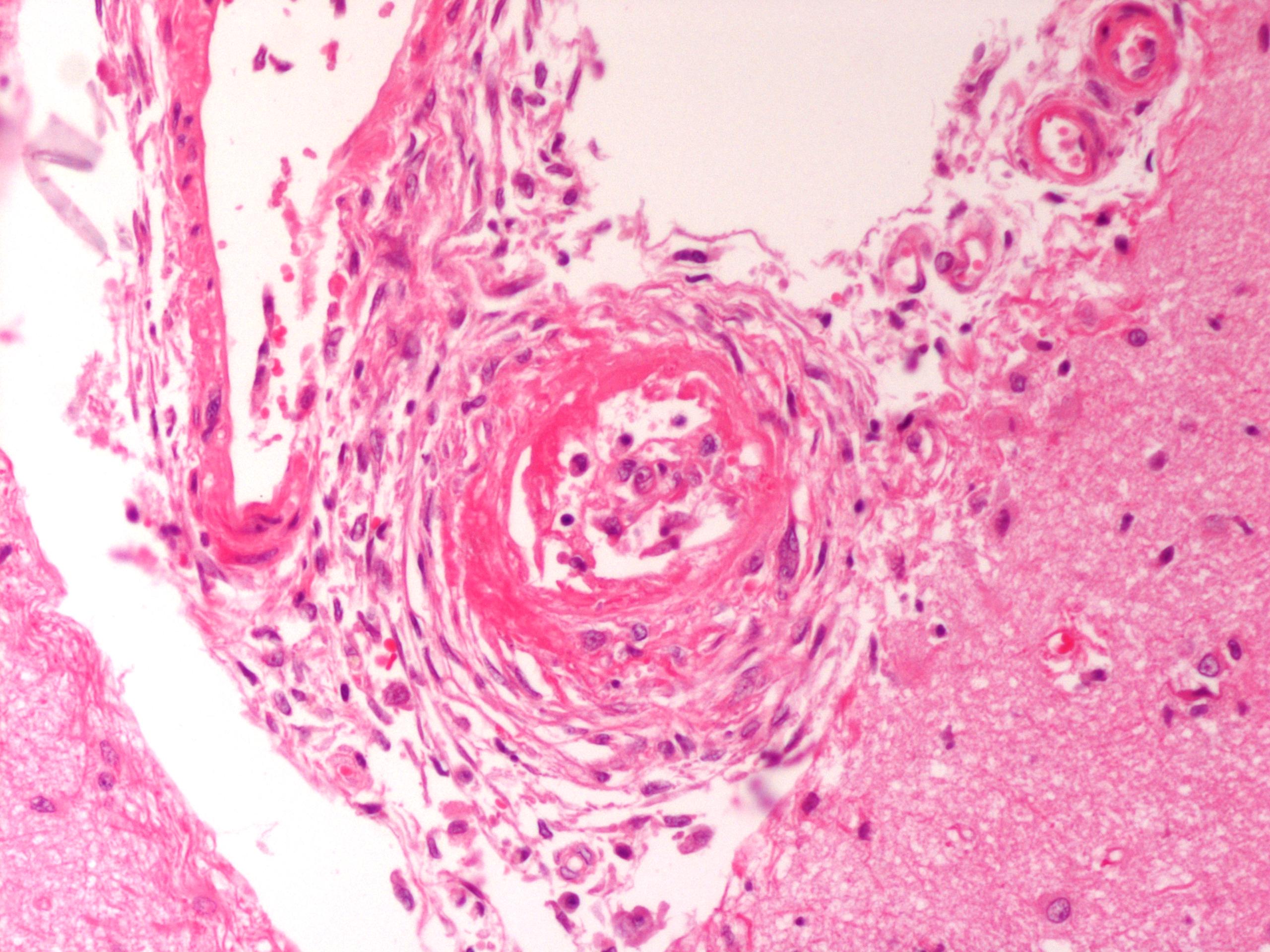
2. Fibrinoid necrosis and adventitial hyperplasia, multifocal, arteries, meninges.
Condition:
Contributor Comment:
The pathogenesis of hypertensive encephalopathy is thought to involve the development of vasogenic edema as a result of sudden increases in blood pressure that exceed the autoregulatory capacity of the vasculature in the brain resulting in endothelial injury and breakdown of the blood- brain barrier.2 The edema is primarily in the white matter where it results in separation of axons and myelin sheaths and pallor of the tissue. There is sometimes increased perivascular space around white matter vessels. Vascular changes, usually in the pia, are consistent with hypertension and include onion-skinning of the vessels (hyperplastic arteriosclerosis) and, occasionally, fibrinoid or hyaline change (hyaline arteriosclerosis).
JPC Diagnosis:
1. Brain,cerebrum,whitematter:Edema, diffuse, moderate, with reactive astrocytosis.
2. Brain, meninges: Hyaline vascular necrosis, multifocal, moderate with perivascular sclerosis.
Conference Comment:
In general, there are four mechanisms of edema:(4)
- Increased microvascular permeability (e.g. vasculitis secondary to endotoxemia)
- Increased intravascular hydrostatic pressure (e.g. pulmonary hypertension)
- Decreased intravascular osmotic pressure (e.g. protein-losing nephropathy/enteropathy)
- Decreased lymphatic drainage (e.g. intestinal lymphangectasia)
McGavin and Zacharys Pathologic Basis of Veterinary Disease expands the mechanistic list by including hydrostatic (interstitial) and hypo-osmotic types of brain edema. Briefly, hydrostatic edema is characterized by extracellular periventricular fluid accumulation as a result of increased hydrostatic pressure within the ventricles. Hypo- osmotic edema occurs with water and salt intoxication in which the differences in osmotic pressure between the brain and the plasma results in movement of fluid from the vasculature into the brain.(5)
In this case, partial herniation of the cerebellum through the foramen magnum (colloquially referred to as cerebellar coning) was noted at necropsy. In addition to the foramen magnum, there are two other potential locations of herniation during brain swelling. The occipital cortex may herniate caudally beneath the tentorium cerebelli or, in cases of unilateral swelling, the cingulate gyrus of the unaffected hemisphere may be forced laterally under the falx cerebri.(4)
Participants also discussed the differential diagnosis for white matter spongiosis, which can be broadly classified as either idiopathic or toxic/metabolic. A more detailed discussion of the various idiopathic spongiform myelinopathies is available within the selected references.(3,4) Toxic and metabolic causes of status spongiosis include, but are not limited to, hepatic encephalopathy, renal encephalopathy, branched chain α-ketoacid decarboxylase deficiency (i.e. maple syrup urinary disease), hexachlorophene toxicosis, halogenated salicylanilide toxicosis, bromethalin toxicity and several plant species.(3)
Chart 1.
| | Vasogenic Edema | Cytotoxic Edema |
| Pathogenesis | Damage to cerebral vasculature → fluid and proteins leave vessel under hydrostatic pressure → edema | Glial cell injury → disturbed cellular osmoregulation → acute cell swelling with maintenance of vascular integrity |
| Gross findings | Flattened gyri and narrowed sulci Herniation (i.e. cerebellar coning) Edematous swelling of the white matter | Similar to findings in vasogenic edema with possible displacement May be grossly normal |
| Distribution of the edema | White matter; may affect grey matter if severe | Grey matter White matter Both |
| Histologic findings | Generalized pallor Swelling and necrosis of astrocytes Astrocyte hypertrophy Eosinophilic lakes of edema fluid |
Astrocyte swelling White matter spongiosis (if oligodendrocytes affected) Intracellular fluid accumulation |
References:
2. Kent M. The cat with neurological manifestations of systemic disease; key conditions impacting on the CNS. Journal of Feline Med Surg. 2009;11:395-407.
3. Maxie MG, Youssef S. Nervous system. In: Maxie MG, ed. Jubb, Kennedy and Palmers Pathology of Domestic Animals. 5th ed., vol. 1. Philadelphia, PA: Elsevier Ltd; 2007:385-388.
4. Summers BA, Cummings JF, de Lahunta A. Principles of neuropathology. In: Veterinary Neuropathology. St. Louis, MO: Mosby; 1995:36-36.
5. Zachary JF. Nervous system. In: McGavin MD, Zachary JF, eds. Pathologic Basis of Veterinary Disease. 4th ed. St. Louis, MO: Elsevier; 2007:862-865.