Signalment:
Gross Description:
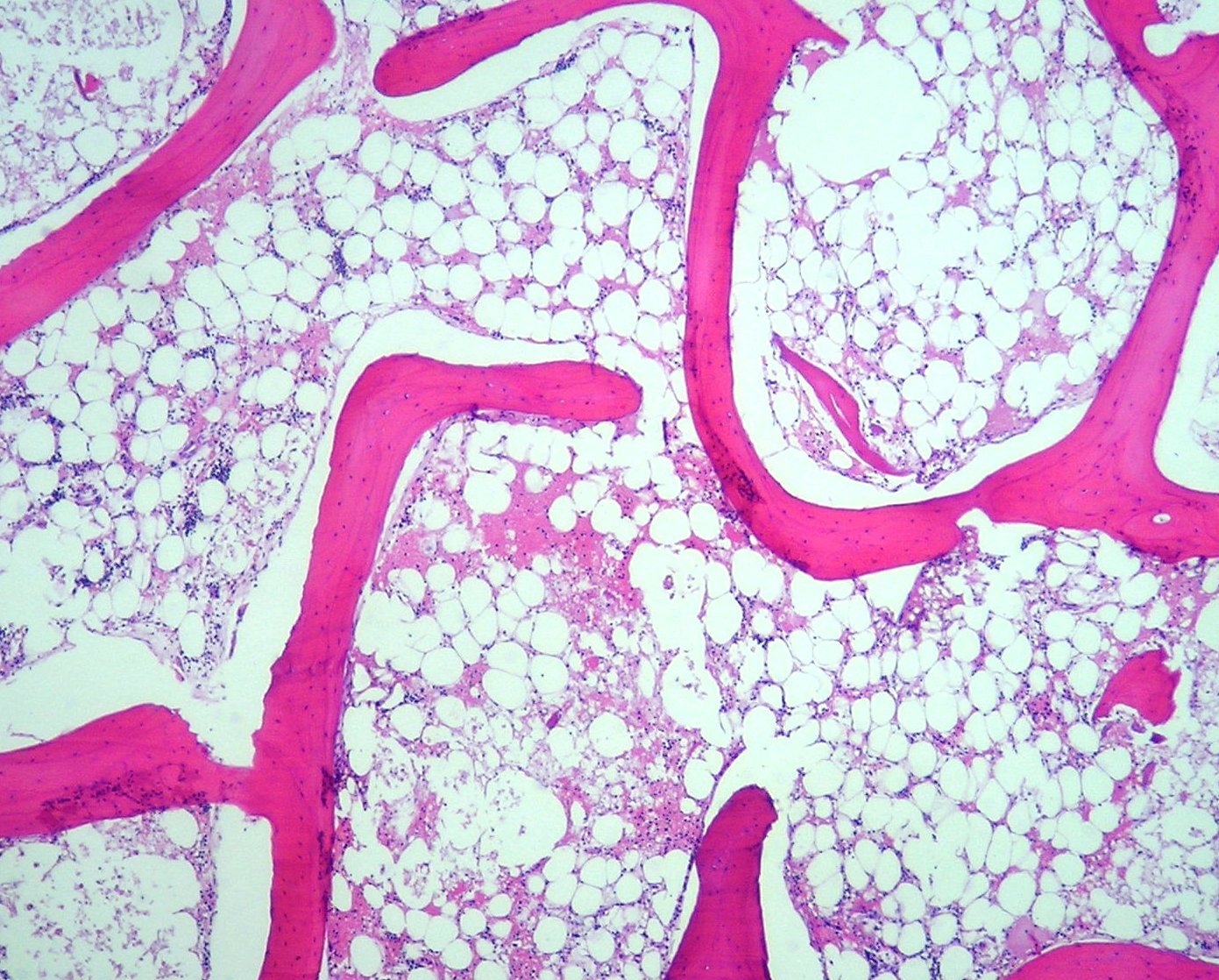
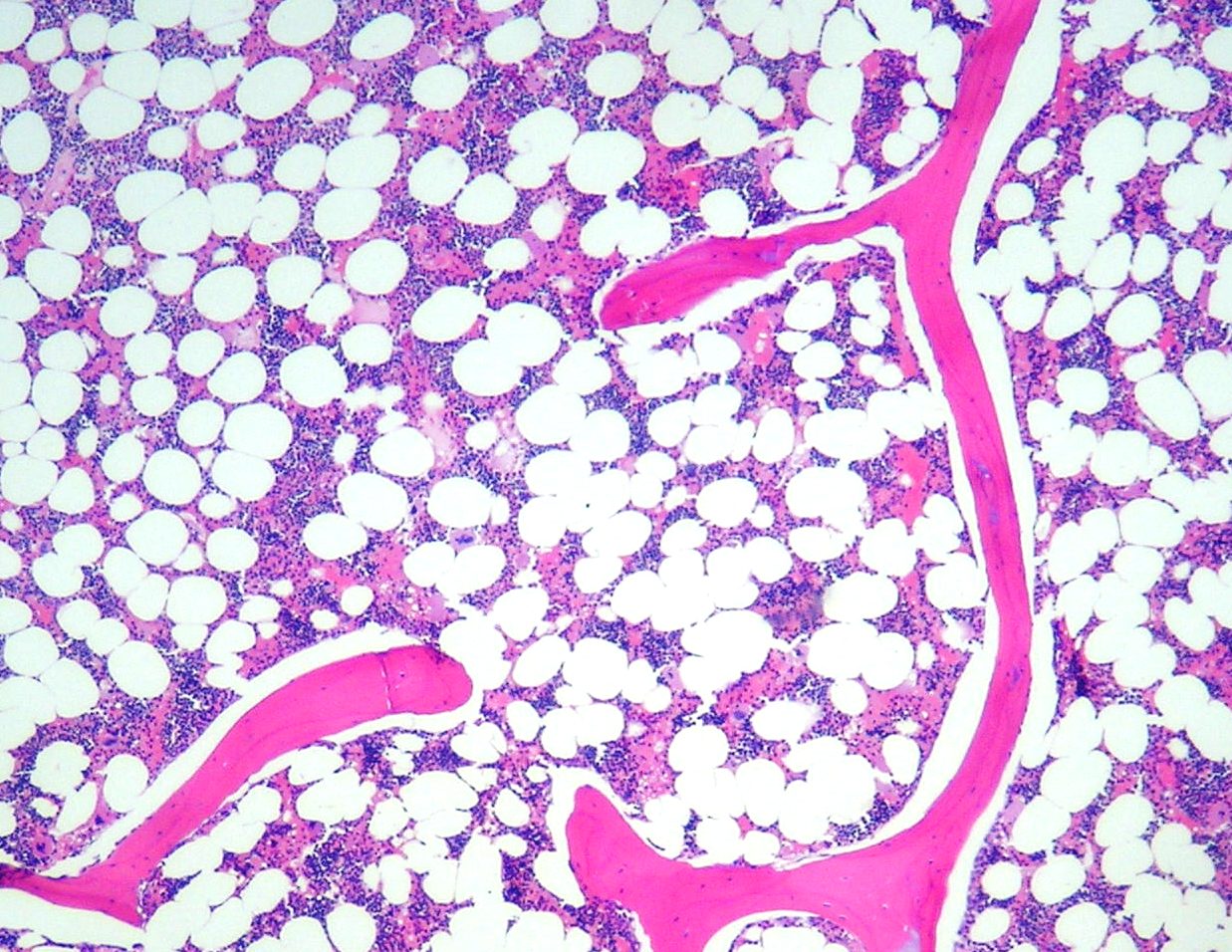
Histopathologic Description:
Morphologic Diagnosis:
Bovine, bone marrow, sternum, aplasia, severe,
Etiologic diagnosis: toxic bone marrow aplasia
Etiology: toxic substance(s) in Pteridium aquilinum
Condition: acute poisoning by Pteridium aquilinum
Lab Results:
| Blood coagulation test | |||
| Parameter | Unity | Reference Values | Affected Bovine |
| Partial time of activated thromboplastin | seg | 25-45 | 49.3 |
| Prothrombin time | seg | Â | 20.2 |
| Complete blood cell count | |||
| Parameter | Unity | Reference Values | Affected Bovine |
| Red blood cells | (x106/mm3) | (5.0-10.0) | 5.1 |
| Hemoglobin | (g/dl) | (8.0-15.0) | 79 |
| Packed cell volume | (%) | (24-46) | 23 |
| Mean corpuscular volume | (fl) | (40.0-60.0) | 45.1 |
| Mean corpuscular hemoglobin concentration | (%) | (30.0-36.0) | 34.3 |
| Leucocytes | (/mm3) | (4,000-12,000) | 5100 |
| Neutrophils | (%) | (15%-45%) | 0 |
| Â | (/mm3) | (600-4,000) | 0 |
| Lymphocytes | (%) | (45%-75%) | 100 |
| Â | (/mm3) | (2,500-7,500) | 5100 |
| Monocytes | (%) | (2%-7%) | 0 |
| Â | (/mm3) | (25-840) | 0 |
| Eosinophils | (%) | (0%-20%) | 0 |
| Â | (/mm3) | (0-2,400) | 0 |
| Basophils | (%) | (0%-2%) | 0 |
| Â | (/mm3) | (0-200) | 0 |
| Platelets | (x103/mm3) | 100-800 | 3 |
Condition:
Contributor Comment:
Clinical signs associated with acute form of bracken fern poisoning in cattle include high fever (up to 42.5°C), severe hemorrhages in various tissues and organs, neutropenia and thrombocytopenia.(4,8,10,15,16) High fever appears to be the first clinical sign of the disease, and some believe (14) the intensity of fever that occurs in acute bracken fern poisoning is not duplicated by any other diseases in cattle. Fever is followed by hemorrhage through nasal cavity and depression. In the advanced stages of the disease the fever may subside.(4,9,10,12)
Acute bracken fern poisoning in cattle has been subdivided by some (10, 12) into two types: 11) enteric, which is the most common and characterized mainly by depression, anorexia, high fever, and weak pulse, blood clots in the feces and foul smelling feces, pale mucous membranes and bleeding from mucous membranes of the nose, eyes, vagina, and anus; and 2) laryngeal-�-�with clinical signs including high fever, roaring, laborious breathing and edema of the larynx. In our experience, however, it is not uncommon to observe signs of both types overlapping in the same animal, as is the case of the bovine of this report. Hemorrhages from venipunctures, from insect bites and in the milk are commonly observed. Death ensues usually 2-3 days after the first clinical signs; however peracute cases of 4-10 hours and cases of recovery are also reported.(4,17) In our region (unpublished data) acute bracken fern poisoning generally occurs in spring and summer months, in hill camps where the ecology is conducive of fern growth, with morbidity rates of 12.5%-21.5% and high lethality rates.
The primary lesion in the acute bracken fern poisoning in cattle is a severe suppression (aplasia) of the bone marrow (as observed in the bovine of this report) which results in thrombocytopenia and neutropenia. No changes are observed in red blood cells (9) and any deficit in RBCs numbers are due more to the hemorrhaging than to the bone marrow suppression since the RBC half-life in cattle is considerably greater (157-162 days) than that of platelets (5-10 days) and neutrophils (12 hours). Usually death due to bleeding related to thrombocytopenia occurs when the numbers of platelets are lower than 10,000/mm3 of blood. In these cases fatal bleeding within body cavities occurs. In the case of this report platelets were 3,000/mm3 one day before death.
There is usually bacteremia related to the almost complete lack of neutrophils in the peripheral blood.(4,9) If after the onset of the bacteremia the bovine survives for several days, infarcts may occur in the liver, lung, kidney and spleen. Death occurs because of internal hemorrhage or septicemia.(10,12)
The most remarkable necropsy findings are hemorrhages of almost any size in almost any organ.(10,12,15) Petechiae and ecchymosis occur in the subcutaneous tissue and there is edema and hemorrhages in lymph nodes; petechiae and paint-brush hemorrhages are observed on serosal surfaces of several organs from abdominal and thoracic cavities. Abundant collections of partially clotted blood can be found in the peritoneal cavity. Mucosal ulcerations and blood clots in the lumen of fore stomachs, abomasum, small and gross intestine are observed. Pale necrotic areas of necrosis can usually be observed in the liver but also in the heart, kidney and spleen. These areas are usually referred to as infarcts but probably are caused by toxins of bacteria and not really by ischemia due to compromise of the vasculature. Pharyngeal and laryngeal edema can be marked.(10,12,16)
The hemorrhages observed grossly can be confirmed histologically. Additionally, foci of coagulative necrosis associated with clusters of bacteria can be found in the liver, heart, kidney and spleen. The most striking histological change is the severe aplasia of the bone marrow.(4,9)
The norsesquiterpene glucoside ptaquiloside is the toxin in P. aquilinum responsible for the bone marrow suppression in acute disease (6); this toxin has cumulative properties and the time elapsed from the beginning of the ingestion of the plant and the development of the clinical signs will depend of the amount of ingested plant.(4,12) Usually the ingestion of daily amounts equal to or above than 10 g/kg/bw during 2-11 weeks are necessary to produce the disease.(4,9)
The list of differential diagnosis for acute bracken fern poisoning in cattle should include anaplasmosis, pneumonic mannheimiosis (differential for the laryngeal form), septicemia pasteurellosis, leptospirosis, sweet clover poisoning, bacillary hemoglobinuria.(12) A similar disease caused by bone marrow suppression is reported in cattle from Australia and is caused by the ingestion of an yet different poisonous plant (Cheilanthes sieberi).(3)
JPC Diagnosis:
Conference Comment:
There are numerous toxins within bracken fern including quercetin, ptaquiloside, shikimic acid, aquilide A, and prunasin.(7,8,19) The two major syndromes commonly seen in cattle are aplastic anemia and enzootic hematuria. The severity of disease depends upon how much of the plant is ingested. There is a cumulative affect with this poison. Morbidity is low and mortality is high with this disease. If enough of the toxin is ingested over weeks to months, death via thrombocytopenic hemorrhage or septicemia secondary to neutropenia is often the result.(7,8,19)
In cattle and sheep, bracken fern poisoning results in an irreversible trilineage marrow hypoplasia and resultant aplastic pancytopenia. The chronic form is usually from long term, low level ingestion of bracken fern resulting in persistent hematuria and alimentary tract neoplasia.(7,8,19) Bracken fern toxicity also commonly causes neoplasia within the urinary bladder.(7,8,19) Papillomas, fibromas, and hemagiomas are most common in the urinary bladder.Â
Hemorrhages can be found in almost any tissue with bracken fern poisoning, but they are usually most numerous in the stomach and small intestine. Multiple neoplasms of the bladder wall or esophagus and forestomachs may also been seen at necropsy. Marrow cellularity is often markedly diminished and the marrow appears pink and soft.(7,8,19)
References:
2. Bosshart JK, Hagan WA: A fatal unidentified disease of cattle in New York State. Cornell Vet 10:102-13,1920
3. Clark IA, Dimmock CK: The toxicity of Cheilanthes sieberi to cattle and sheep. Aust Vet J 47:149-152, 1971
4. Evans WC, Evans ET, Hughes LE: Studies on bracken poisoning. Part III. Field outbreaks of bovine bracken poisoning. Brit Vet J 110:426-442, 1954
5. Hagan WA, Zeissig A: Experimental bracken poisoning of cattle. Cornell Vet 17:194-208, 1927
6. Hirono I, Kono Y, Takahashi K, Yamada K, Niwa H, Ojika M, Kigoshi H, Hiiyama K, Uosaki Y: Reproduction of acute bracken poisoning in a calf with ptaquiloside, a bracken constituent. Vet. Rec. 115:375-378, 1984
7. Maxie MG, Youssef S: Nervous system. In: Jubb, Kennedy, and Palmers Pathology of Domestic Animals, ed. Maxie MG, 5th ed., vol 1, pp. 354-357. Saunders Elsevier, Philadelphia, PA, 2007
8. Maxie MG, Newman SJ: Urinary system: In: Jubb, Kennedy, and Palmers Pathology of Domestic Animals, ed. Maxie MG, 5th ed., vol 2, pp. 518-520. Saunders Elsevier, Philadelphia, PA, 2007
9. Naftalin JM, Cushnie GH: Pathology of bracken fern poisoning in cattle. J. Comp. Path Therap 64:54-74, 1954
10. Osebold JW: An approach to the pathogenesis of fern poisoning in the bovine species. J Am Vet Med Assoc 121:440-441, 1951
11. Rissi DR, Rech RR, Pierezan F, Gabriel AL, Trost ME, Brum JS, Kommers GD, Barros CSL: Plant and plant-associated mycotoxins poisoning in cattle in Rio Grande do Sul, Brazil: 461 cases. [Intoxica+�-�+�-�o por plantas e micotoxinas associadas a plantas em bovinos no Rio Grande do Sul]. Pesq Vet Bras 27:261-268, 2007. (In Portuguese, Abstract in English)
12. Sippel WL: Bracken fern poisoning. J Am Vet Med Assoc 121:9-13, 1952
13. Souto MAM, Kommers GD, Barros CSL, Piazer JVM, Rech RR, Riet-Correa F & Schild AL: Neoplasms of the upper digestive tract of cattle associated with spontaneous ingestion of bracken fern (Pteridium aquilinum). [Neoplasias do trato alimentar superior de bovinos associadas ao consumo