Signalment:
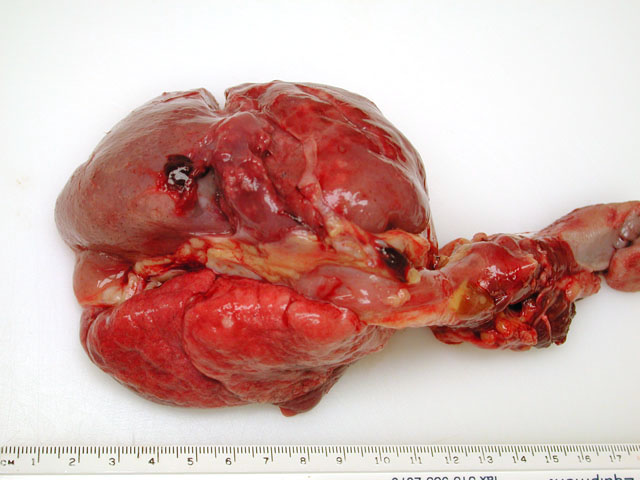
Gross Description:
In addition to the pulmonary lesion, the coronary arteries were segmentally thickened by yellow plaques on the intimal surfaces (atherosclerosis).
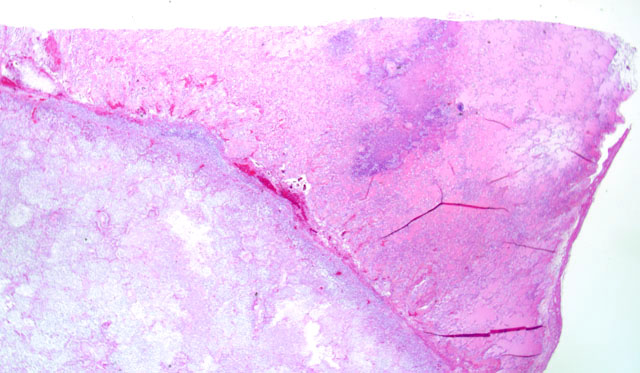
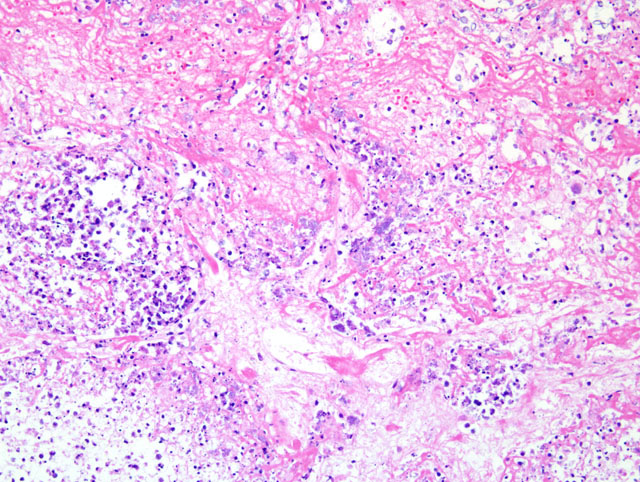
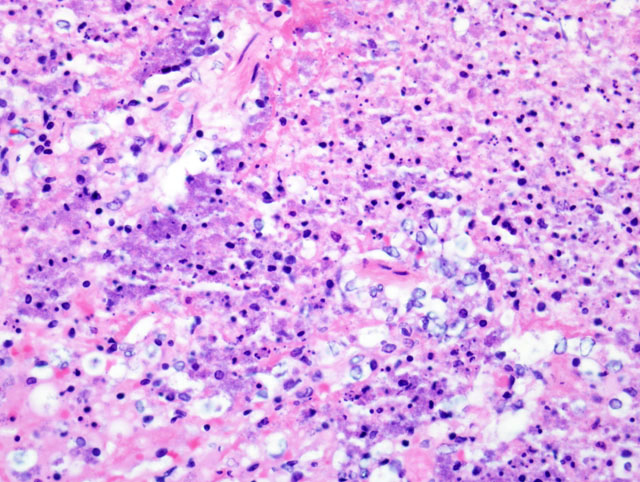
Histopathologic Description:
Morphologic Diagnosis:
Lab Results:
Glucose, 348 mg/dL
BUN 29 mg/dL
K+ 6.2 mEq/L
Alkaline phosphatase 588 μ/L
Cholesterol 1099 mg/dL
Hematology:
CBC:
RBC, 6.77 x 105/μL
Hematocrit, 42.3 %
Hemoglobin, 12 mg/dL
MCV, 62fl
MCHC 28.4 g/dL
Platelets 181 x 103/μL
WBC 15.9 x 103/μL
Neutrophils, 77% (12243)
Bands, 0
Lymphocytes 17% (2703)
Monocytes, 5% (795)
Eosinophils, 1% (159)
Basophils, 0
Microbiology:
Pleural fluid and a lung swab were submitted for bacterial culture. A heavy pure growth (4+) of Corynebacterium ulcerans was recovered.
Condition:
Contributor Comment:
The pathogenicity of C. ulcerans is facilitated by potent exotoxins, including diphtheria toxin which inhibits protein synthesis, as well as necrotizing toxin which increases vascular permeability resulting in edema. After inhalation, C. ulcerans proliferates in the respiratory tract epithelium. Subsequent release of the exotoxins causes epithelial necrosis, which in turn initiates marked interstitial edema, neutrophil infiltration, and fibrinosuppurative exudation.(1)
The differential diagnosis for fibrinosuppurative bronchopneumonia in cynomolgus macaques should include Streptococcus pneumoniae, Pasteurella spp., Nocardia spp., Actinobacillus spp., Klebsiella spp., and Legionella pneumophila as well as Corynebacterium sp.
JPC Diagnosis:
Conference Comment:
Corynebacterium ulcerans can produce diphtheria toxin similar to that of C. diphtheriae. C. diphtheriae produces a phage-encoded A-B toxin that blocks protein synthesis. Even after vaccination with diphtheroid toxin, C. diphtheriae can still colonize the epithelium, and the vaccine does protect people from the harmful effects of the toxin. Release of the exotoxin in unvaccinated individuals causes necrosis of the epithelium and subsequent profuse fibrionsuppurative exudation. The settling of this exudate on the already ulcerated epithelial surface results in formation of the firm diphtheritic membrane characteristic of the disease. If the fulminant infection is stopped, the membrane may be sloughed via coughing or enzymatic digestion, and the patient can recover.(4)
References:
2. Dessau RB, Brandtchristensen M, Jensen OJ, Tonnesen P: pulmonary nodules due to Corynebacterium ulcerans. European Respiratory Journal 8: 651-653, 1995
3. Panaitescu M, Maximescu P, Michel J, Potorac E: Respiratory pathogens in non-human primates with special reference to Corynebacterium ulcerans. Lab Animal 11:155-157, 1977
4. McAdam AJ, Sharpe AH: Infectious Diseases. In Robins and Cotran Pathologic Basis of Disease, ed. Kumar V, Abbas AK, Fausto N, 7th ed., pp. 374, Elsevier Saunders, Philadelphia, PA 2005
5. Sing A, Hogardt M, Bierschenk S, Heesemann E: Detection of differences in the nucleotide and amino acid sequences of diphtheria toxin from Corynebacterium diphtheriae and Corynebacterium ulcerans causing extrapharyngeal infections. Journal of Clinical Microbiology 41: 4848-4851, 2003
6. Wagner J, Ignatius R, Voss S, Hopfner V, Ehlers S, Funke G, Weber U, Hahn H: Infection of the skin caused by Corynebacterium ulcerans and mimicking classical cutaneous diphtheria. Clinical Infectious Diseases 33: 1598-1600