Signalment:
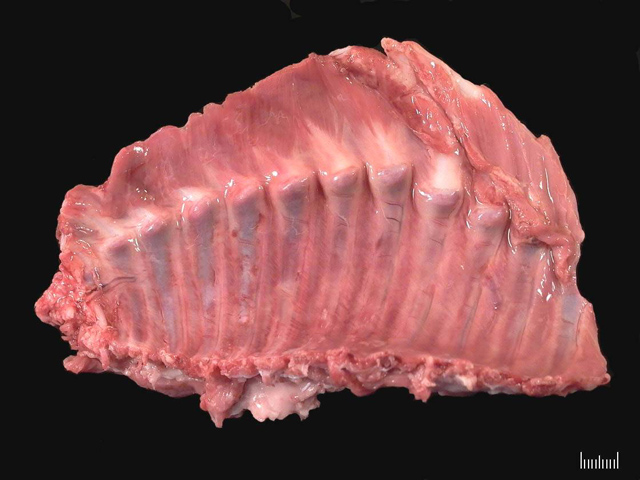
Gross Description:
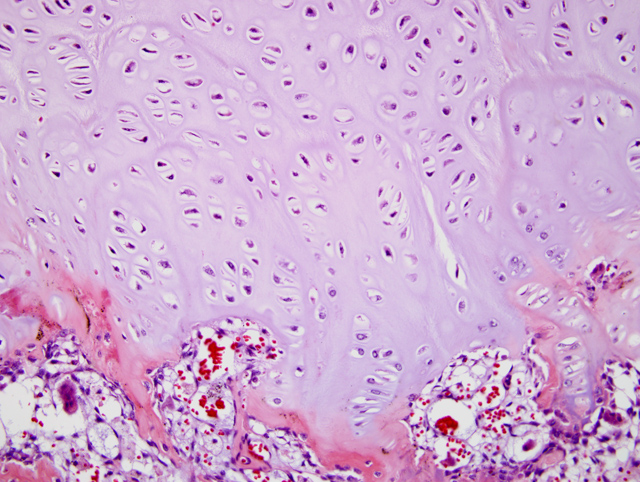
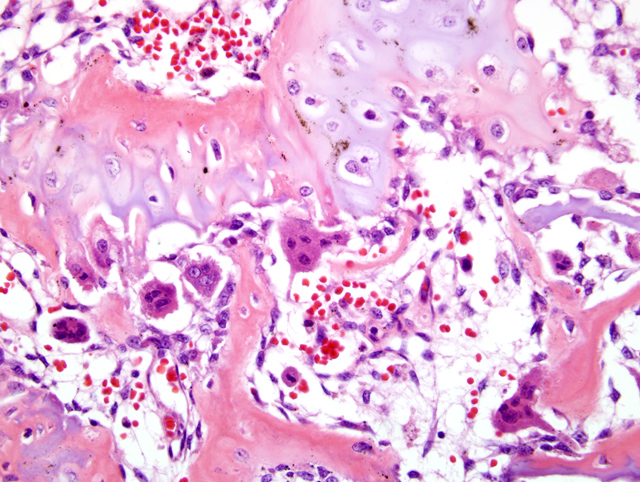
Histopathologic Description:
Morphologic Diagnosis:
Lab Results:
| DateTreatment | Calcium Blood Level (RR 8.6-11.8 mg/dL) |
Parathyroid Hormone Level (RR 27-155 pg/mL) |
||
| Calcitriol (ng/day) | CaCO3 (mg/day) |
|||
| 8-17-07 | N/A | N/A | 5.6 | 782.1 |
| 8-25-07 | 150 | 100 | - | - |
| 9-15-07 | 200 | 250 | 6.0 | - |
| 9-20-07 | 250 | 250 | 5.1 | - |
| 8-17-07 | 350 | 250 | 4.9 | - |
| 10-20-07 | 400 | 300 | 5.7 | 863.8 |
Condition:
Contributor Comment:
Two main forms of vitamin D-resistant rickets are characterized in humans. Type I is an inborn error in conversion of 25-(OH)D3 to 1,25(OH)2D3 due to a deficiency of the renal 1-hydroxylase enzyme. This condition responds to large doses of vitamin D2 and D3. Vitamin D-resistant rickets Type II (VDRR II) in humans is an end organ resistance to 1,25(OH)2D3 due to an autosomal recessive congenital defect in the vitamin D receptor (VDR) or a site distal to it. This type of rickets has been reported in a few cats, (4,5,6) but has never before been reported in a canine. In one of the feline cases the cat had signs of hypocalcemia, including muscle tremors, similar to the clinical signs in this canine patient.(5) Two other cats had similar radiologic changes of the radius and ulna, as in the present case, as well as similar costochondral junction changes.(4,6) Similarly these cases had no response to high levels of vitamin D or calcium supplementation; (4,6) however, in two of the cases, the cats became normal after physeal closure.(4,5)
Three main intracellular defects have been identified in human cases of VDRR II:
- Hormone binding defects including decreased number of sites, decreased binding affinity, or complete absence of binding.
- Deficient nuclear localization in these cases there is normal binding affinity and capacity, but unmeasurable localization to the nucleus.Â
- A post-receptor defect characterized by normal receptors but deficiency in the induction of the 25-(OH)D-24 hydroxylase enzyme in response to 1,25(OH)2D.(3)
Defects can be detected using in vitro assessment of VDR binding or the subsequent cellular response to VDR binding by 1,25 dihydroxycholecalciferol (1,25(OH)2D) in cells, typically fibroblasts cultured from skin biopsies, derived from individuals affected by clinical signs of VDRR II and compared with normal controls.(4) A diagnosis of VDRR II was made in the present case based on clinical signs, radiographic findings, biochemistry, parathyroid levels, and the inability of fibroblasts from the skin of the dog to bind 1,25(OH)2D. A vitamin D receptor defect was verified through genetic testing on cultured fibroblasts from this dog at Stanford University, confirming the diagnosis of VDRR II in this patient.Â
This patient also presented with generalized alopecia, as is the case in approximately 50% of human cases of VDRR II.(3) Keratinocytes contain vitamin D receptors and can respond to the 1,25(OH)2D3 produced. The alopecia found in VDR deficient patients suggests a biologic role for the VDR in the epidermis, particularly in the hair follicle.(8) In VDR knock out mice models, the mice are fully haired and grossly normal after birth until approximately three months of age, progressing to generalized alopecia by eight months of age.(8) These findings indicate that the prenatal hair growth and development of the epidermis and first hair growth cycle does not require VDR, but is important in the onset of the second hair growth cycle.(8) Examination of the skin in this canine patient revealed large cystic follicles filled with keratin which corresponds to dermal changes noted in human cases and in rodent models of the disease.(8)
Humans with VDRR II, as well as the patient in this case, are born with normal hair, but become alopecic by six months of age and have rachitic changes that are resistant to all forms of vitamin D therapy.(1) Alopecia generally does not improve in human patients, (1) but normal pelage returned in our canine patient after several months. It is not clear if the alopecia is a genetically linked abnormality or related to the effect of 1,25(OH)2D3 on the hair follicle.(1) In humans, alopecia seems to be a marker of a more severe form of the disease as judged by the earlier age at presentation, marked clinical aberrations and poor response to therapy.(3)
Therapy in humans begins with very large doses of vitamin D and oral calcium supplements but has had limited success. Refractory cases need long term nocturnal intravenous calcium infusions and these have successfully healed rickets and promoted mineralization in these patients; (2) however, the therapy is cost prohibitive in veterinary cases.
JPC Diagnosis:
Conference Comment:
Hypophosphatemia can lead to rickets, and is known as hypophosphatemic vitamin D-resistant rickets (renal hypophosphatemic rickets).(7) Hypophosphatemia, normocalcemia, and decreased renal tubular reabsorption of phosphate are characteristic of hypophosphatemic vitamin D-resistant rickets. Hypophosphatemia is the sequela of inadequate absorption of phosphorus from the gastrointestinal system or decreased/inadequate reabsorption of phosphorous from the renal system.(7)
Gross lesions of rickets are most striking at sites of rapid growth. The metaphyseal and epiphyseal regions of long bones and the costochondral junctions are commonly affected, producing the classic rachitic rosary in affected animals.(7)
The classic histologic appearance of rickets is the disorganization of columns of chondrocytes and persistence of hypertrophic chondrocytes at sites of endochondral ossification, both at the physes and beneath the articular cartilage.(7) The underlying trabecular bone is often disrupted, and irregular tongues of cartilage are often seen in the metaphyses due to disorganized and disrupted endochondral ossification.
References:
2. Avioli LV and Krane SM: Metabolic Bone Disease and Clinically Related Disorders, 3rd ed., pp. 221, 767-777, Academic Press, San Diego, CA, 1998
3. Favus, MJ: Primer on the Metabolic Bone Diseases and Disorders of Mineral Metabolism, 3rd ed., pp. 311-316, Lippincott-Raven, Philadelphia, PA, 1996
4. Godfrey DR, Anderson RM, Barber PJ, Hewison M: Vitamin D-dependent rickets type II in a cat. J Small Anim Pract 46:440-444, 2005
5. Schreiner CA, Nagode LA: Vitamin D-dependent rickets type 2 in a four-month old cat. JAVMA 222:337-339, 2003
6. Tanner E, Langley-Hobbs SJ: Vitamin D-dependent rickets type 2 with characteristic radiographic changes in a 4-month-old kitten. J Feline Med Surg 7:307-311, 2005
7. Thompson K: Diseases of bones and joints. In: Jubb, Kennedy, and Palmer's Pathology of Domestic Animals, ed. Maxie MG, 5th ed., vol. 1, pp. 75-82. WB Saunders, Edinburgh, Scotland, 2007
8. Xie Z, Komuves L, Yu Q-C, Elalieh H, Ng DC, Leary C, Chang S, Crumrine D, Yoshizawa T, Kato S, Bikle DD: Lack of the vitamin D receptor is associated with reduced epidermal differentiation and hair follicle growth. J Invest Dermatol 118:11-16, 2002