Signalment:
6-month-old, intact male, Dalmation, CanineChronic intermittent vomiting with a recent history of hematemesis and melena. Patchy alopecia on face, left elbow, and right foot
Gross Description:
Exploratory surgery revealed multiple acquired extrahepatic shunts. The liver had a greenish tint and accentuated lobular pattern.
Histopathologic Description:
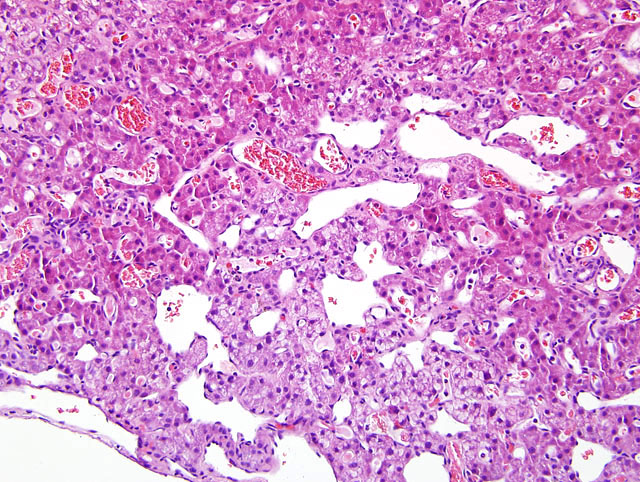
Widespread ectasia and reduplication of portal and central veins is prominent. The venous tunics are thickened by a combination of smooth muscle and fibrous connective tissue. Prominent vascularization and occasional arteriolization of hepatic sinusoids is apparent
(fig. 1-1). Scattered mixed inflammatory cellular infiltrates are seen in portal and central areas. Centrilobular hepatocytes exhibit variable cell swelling and degeneration. Increased apoptotic bodies and hepatocellular pigmentation is also seen. There is extensive distension of subcapsular lymphatics and/or veins.
Morphologic Diagnosis:
Liver, severe microvascular dysplasia
Lab Results:
Patient values are followed by reference interval. Anemia: Erythrocytes [3.15 (5.4-8.4)], Hemoglobin [6.9 (12-18)], Hematocrit [20.3 (35-54)], mild neutrophilia and monocytosis - increased ALP [620 (0-100)], ALT [172 (0-60)], AST [100 (0-50)], total bilirubin [0.7 (0.0-0.4)] and cholesterol [364(150-240)], prolonged PTT [24.4 (9.0-12.0)]. Hyperechoic enlarged liver and enlarged gall bladder on ultrasound.Â
Hepatic copper levels were 459 ppm.
Condition:
Microvascular dyplasia
Contributor Comment:
Hepatic microvascular dysplasia (HMD) is a syndrome of young to middle aged dogs, which present with signs of liver failure. The most common signs are CNS signs, vomiting, and/or diarrhea. The major differential diagnosis, both clinically and histopathologically, in the younger dogs is portosystemic shunts. In this case, the diagnosis of HMD was made primarily on the basis of the prominent vascularization of the hepatic sinusoids. Additionally, the dilation of the portal veins and minimal duplication of portal arterioles favors HMD over portosystemic shunt. The dilation of portal veins is presumed (though not proven in the literature reviewed by the submitter) to arise from portal hypertension, which could cause the secondary development of extrahepatic shunts as seen in this case.Â
Yorkshire terriers and Cairn terriers have higher incidence of HMD, but it has been reported in numerous breeds. There are two hypotheses proposed for the cause of HMD. First is that the persistence of embryonic vitelline veins causes intrahepatic micro-shunts from the portal veins to the central veins. The other is that ultrastructural defects in the sinusoids cause reduced sinusoidal permeability and limited access of plasma components to the hepatocellular surfaces. The prognosis for uncomplicated HMD is better than that of portosystemic shunts. Many respond to dietary management alone and may survive for more than 5 years in good to excellent clinical condition.
JPC Diagnosis:
1. Liver: Venous dilation, portal and
central, diffuse, with lymphangiectasia, mild arteriolar
and biliary reduplication, multifocal dissecting fibrosis,
sinusoidal ectasia and capillarization, lobule atrophy,
multifocal centrilobular hepatocellular degeneration and
necrosis, and lipogranulomas, Dalmation (Canis familiaris),
canine.
2. Liver: Hepatitis, neutrophilic, multifocal, mild.
Conference Comment:
The process appears centered on the sinusoids with sinusoidal
capillarization and possibly expanded basement
membranes beneath them. Given the loss of lobular architecture,
scattered mild fibrosis, mild inflammation,
individual cell necrosis and pigment accumulation, this
may be an example of lobular dissecting hepatitis in resolution
with secondary portal hypertension. Lobular dissecting
hepatitis, a form of cirrhosis of unknown etiology
reported in young dogs, is characterized by dissection of
the lobular architecture by fibroblasts and thin strands of
extracellular matrix into small groups of hepatocytes,
with accompanying mild to moderate inflammation and
hepatocellular apoptosis or necrosis.
2
Hepatic microvascular dysplasia is a poorly characterized
condition with often confusing or contradictory descriptions
in the literature on the disease etiology, description,
and pathogenesis. The most current characterization,
provided by the World Small Animal Veterinary Association
(WSAVA) Working Group on Liver Disease and
published in 2006, describes the condition as being no
different from primary portal vein hypoplasia. The group
prefers the latter term as more descriptive of the disease
process.
2 Histologically, portal vein hypoplasia shares
many features with congenital portosystemic shunts, intrahepatic
arterioportal fistulas, and portal vein obstruction,
including absent or diminished portal vein profiles
and increased numbers of arteriolar profiles.
2 This standard
was published after the submission of this case as a
Wednesday Slide Conference submission, so this classification
was not available for inclusion in the contributors
comments.
We thank Dr. John Cullen, Dr. Yvonne Schulman, and
Dr. Thomas Lipscomb for their review and consultation
of this case.
References:
1. Christiansen JS, Hottinger HA, Allen L, Phillips L, and Aronson LR: Hepatic microvascular dysplasia in dogs: a retrospective study of 24 cases (1987-1995). J Am Anim Hosp Assoc 36:385-389, 2000
2. Cullen JM, van den Ingh TSGAM, Bunch SE,
Rothuizen J, Washabau RJ, Desmet VJ: Morphological
classification of the circulatory disorders of the canine
and feline liver. In: WSAVA Standards for Clinical and
Histological Diagnosis of Canine and Feline Liver Diseases,
pp 51-52; 97-98. Elsevier Limited, St. Louis, MO, 2006
3. Phillips L, Tappe J, Lyman R, Dubois J, Jarboe J: Hepatic
microvascular dysplasia in dogs. Prog Vet Neurol
7:88-96, 1996
4. Schermerhorn T, Center SA, Dykes NL, Rowland PH,
Yeager AE, Erb HN, Oberhansley K, Bonda M: Characterization
of hepatoportal microvascular dysplasia in a
kindred of cairn terriers. J Vet Intern Med 10:219-
230,1996