Signalment:
Gross Description:
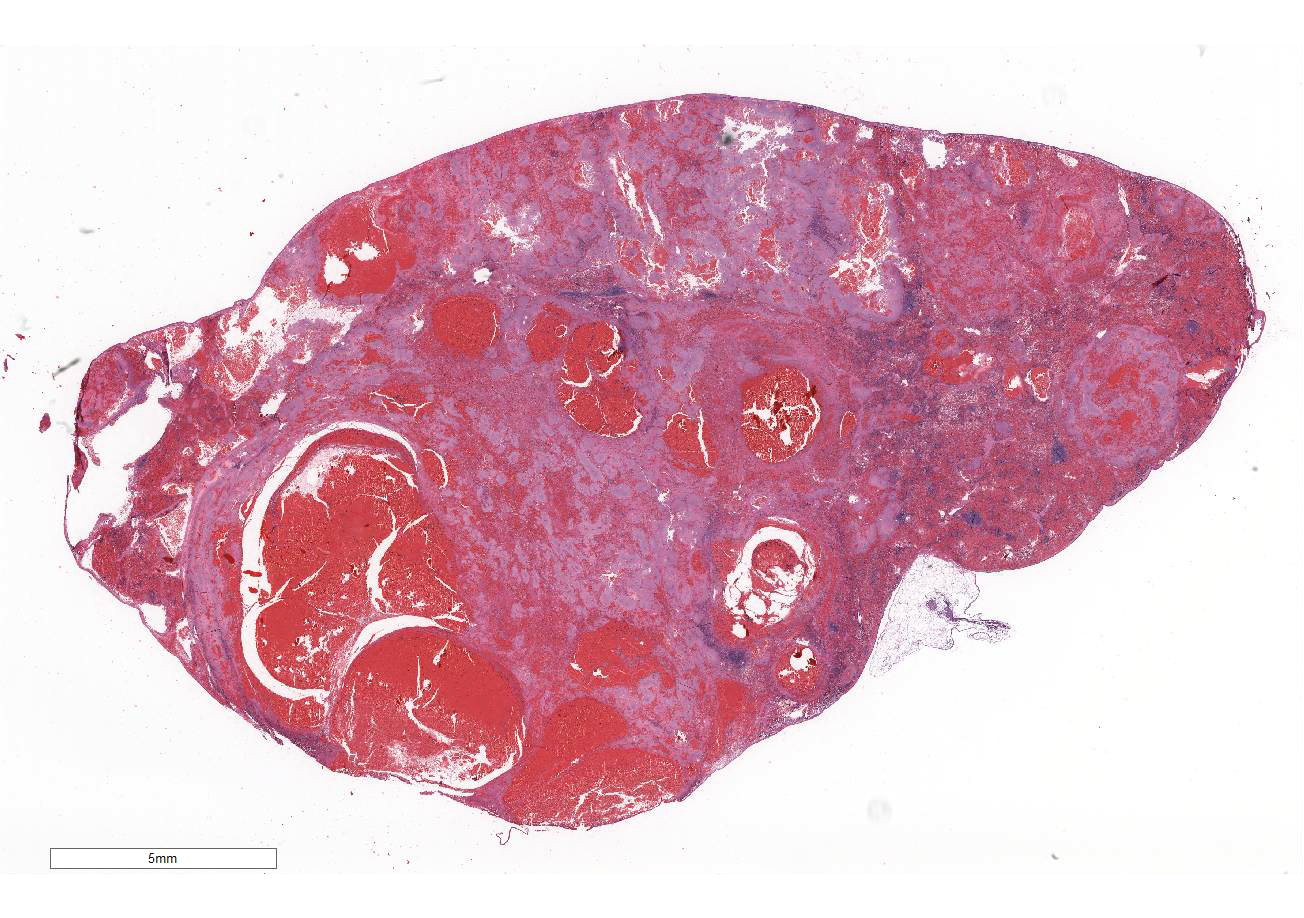
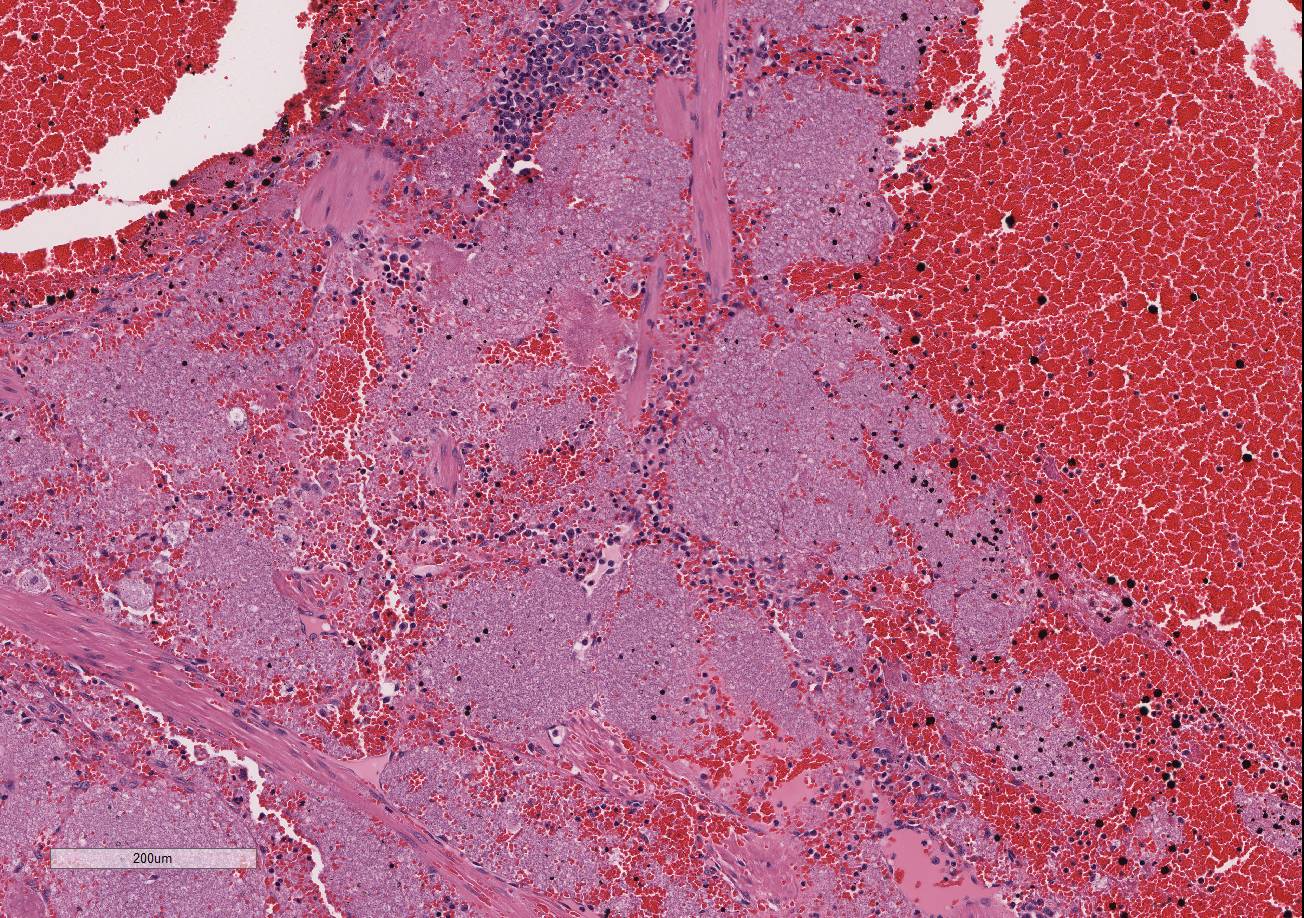
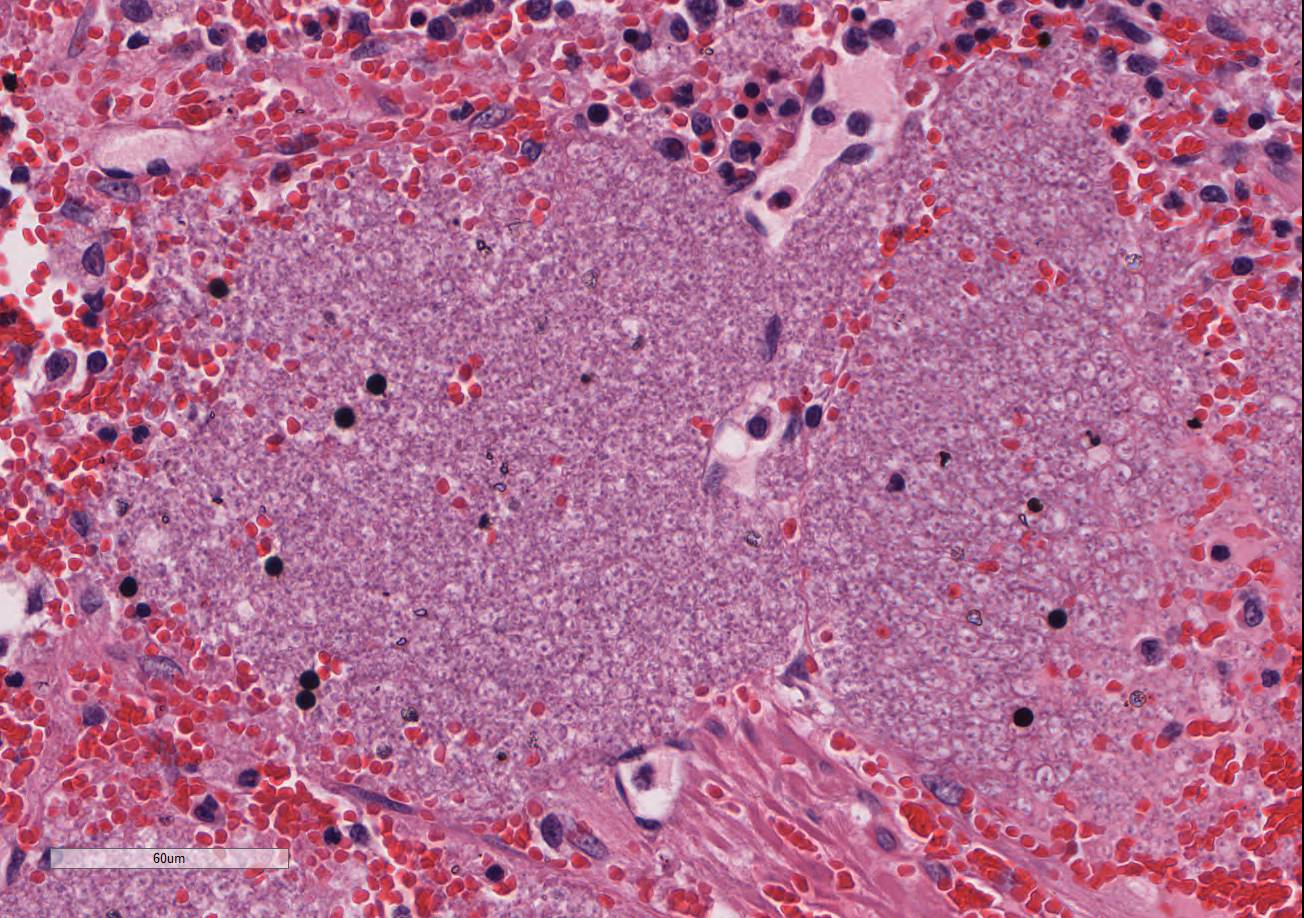
Histopathologic Description:
Morphologic Diagnosis:
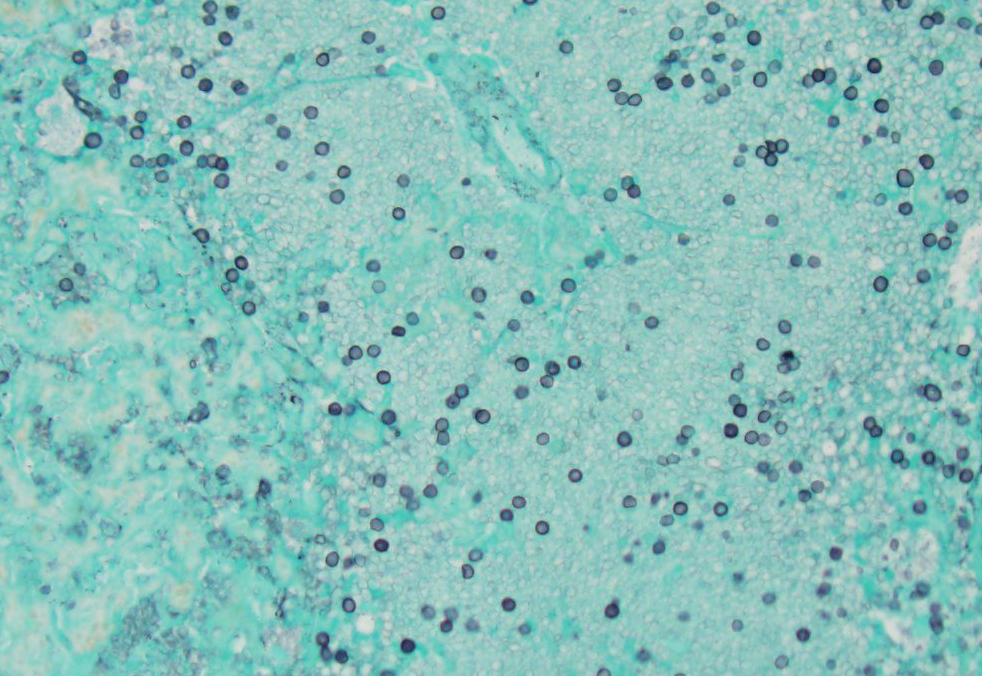
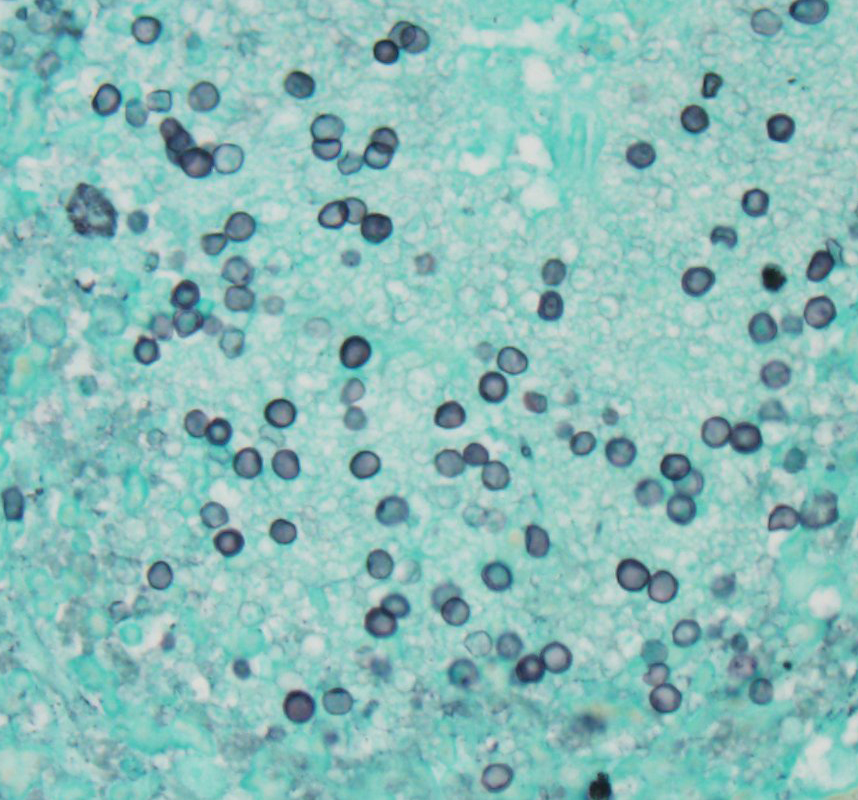
Pneumocystis spp. confirmed with immuno-histochemistry, electron microscopy, and PCR testing. Sequencing suggests a novel species/strain.
Lab Results:
Condition:
Contributor Comment:
Pneumocystis is a saprophytic organism that has somewhat uncertain taxonomy. Pneumocystis has been classified as a unicellular protozoan of the phylum Sarcomastigophora, subphylum Sarcodina. The reproductive behavior is similar to the ascospore formation of yeast cells and the staining properties resemble that of pathogenic fungi. Based on 16S-like rRNA, Pneumocystis is phylogenetically most closely related to the fungi of the class Ascomycetes. Multiple species have been designated, although there is some controversy in this area and several strains likely exist. The most widely referenced species are Pneumocystis carinii in dogs and P. jiroveci in humans, with several species indicated in the laboratory animal literature. The life cycle of Pneumocystis involves a tropho-zoite and a cyst form, both of which occur in the infected tissue.5
Pneumocystis is best known as an opportunistic organism that most commonly causes pneumonia, in particular in immuno-compromised people and animals. Clinical pneumonia occurs in many cases, but subclinical or latent infections are also common in many animal species, including cats. Clinical disease may occur via new infection or reactivation of a latent infection under conditions of stress, immuno-suppressive therapy, or with other underlying infection, such as canine distemper virus in dogs.5 In dogs, most reported cases of pneumocystic pneumonia occur in animals with underlying immuno-deficiency, such as miniature Dachshund, Pomeranian and Cavalier King Charles spaniel dogs with combined immunodeficiency syndrome.2,4 In cats, subclinical or latent infections are most common, and although Pneumocystis has been identified in the lungs in the cat, natural cases of clinical disease have not been reported.5 Under experimental conditions, immunosuppression with glucocorticoid administration has led to pneumocystic pneumonia in cats.5
Extrapulmonary infection with Pneumo-cystis has been reported in humans, particularly with HIV/AIDS, and involves the spleen in some cases.1,3 A case of extrapulmonary pneumocystosis has also been reported in a dog.5 In humans with extrapulmonary infections, some cases have concurrent pneumocystic pneumonia, while others do not, and those that do not are thought to either acquire a primary extra-pulmonary infection or have reactivation of a latent infection at extrapulmonary sites.1 Other than spleen, reported sites for extrapulmonary involvement in humans include lymph node, liver, bone marrow, adrenal gland, gastro-intestinal tract, kidney, thyroid gland, heart, pancreas, central nervous system, bone, eyes or ears.1,3 In a minority of cases, intravascular organisms are identified in the tissues,1 which was present in the liver biopsy from this patient.
In pneumocystic pneumonia, the classic histologic appearance is of intra-alveolar aggregates of foamy eosinophilic material with only a minor infiltrate of macrophages and without significant neutrophilic inflammation. GMS staining highlights the 4-7um diameter cyst wall and more easily demonstrates the ovoid, irregular or crescent shape of the cysts. At extrapulmonary sites, Pneumocystis has similar tissue destruction with necrosis and a similar appearance of foamy eosinophilic material.1,3 Methods of confirmation of Pneumocystis include cytologic or histologic morphologic appearance and GMS staining characteristics, PCR evaluation, immuno-histochemistry or immunofluorescence.3,5
JPC Diagnosis:
Conference Comment:
As mentioned above, extrapulmonary pneumocystosis is rare but has been reported in a dog and immunocompromised people, typically affected with HIV/AIDS.3,5,6 Postmortem analysis from previously reported human cases indicates that Pneumocystis sp. can disseminate throughout the body via hematogenous and/or lymphatic routes. It is thought that the vast majority of cases of extrapulmonary pneumocystosis result from hematogenous or lymphatic spread from the lung. However, in cases where the lungs are unaffected, such as in this cat, there may be reactivation of latent infection in extra-pulmonary organs due to severe immunosuppression.6
References: