Joint Pathology Center
Veterinary Pathology Services
Wednesday Slide Conference
2018-2019
Conference 14
9 January, 2019
CASE I: NE 17-176 (JPC 4101745).
Signalment: 6-year-old neutered male brindle Mastiff dog, Canis familiaris
History: This dog had a 10-minute seizure at home and afterwards he was blind. He had had a similar, but less severe episode of altered mental status several weeks prior. Physical exam findings included dull mentation, circling to the right, and negative menace response. After premedication for imaging, the dog developed ventricular tachycardia and was euthanized.
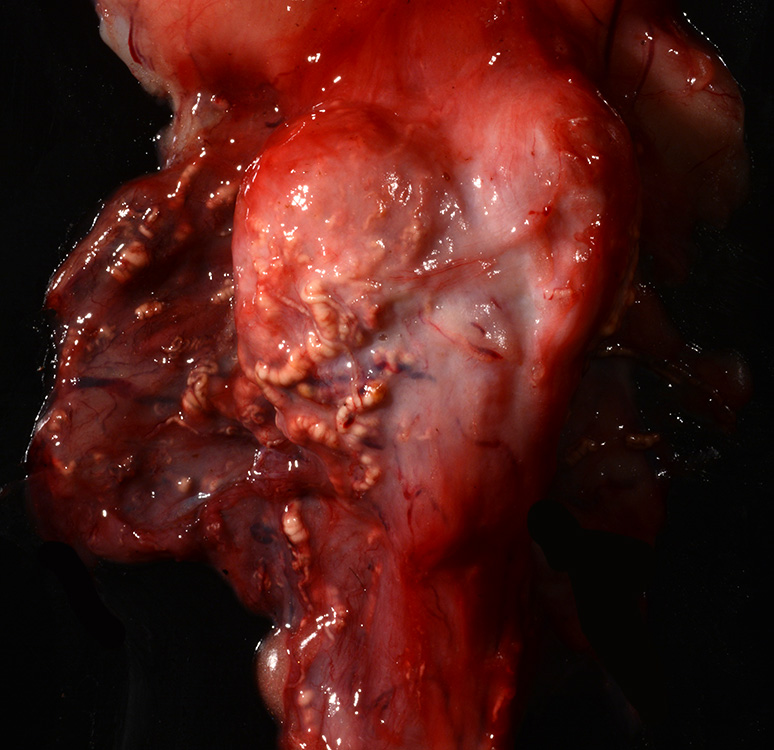
Gross Pathology: The dog was in obese nutritional condition (body condition score 4.5/5) and the tail was alopecic. The thyroid glands were small (right 3x2x32mm; left 5x3x30mm). The walls of many vessels including the coronary arteries, prostatic vessels, and meningeal vessels had white opaque firm walls. The myocardium adjacent to affected coronary vessels was often red.
Laboratory results: None.
Microscopic Description:
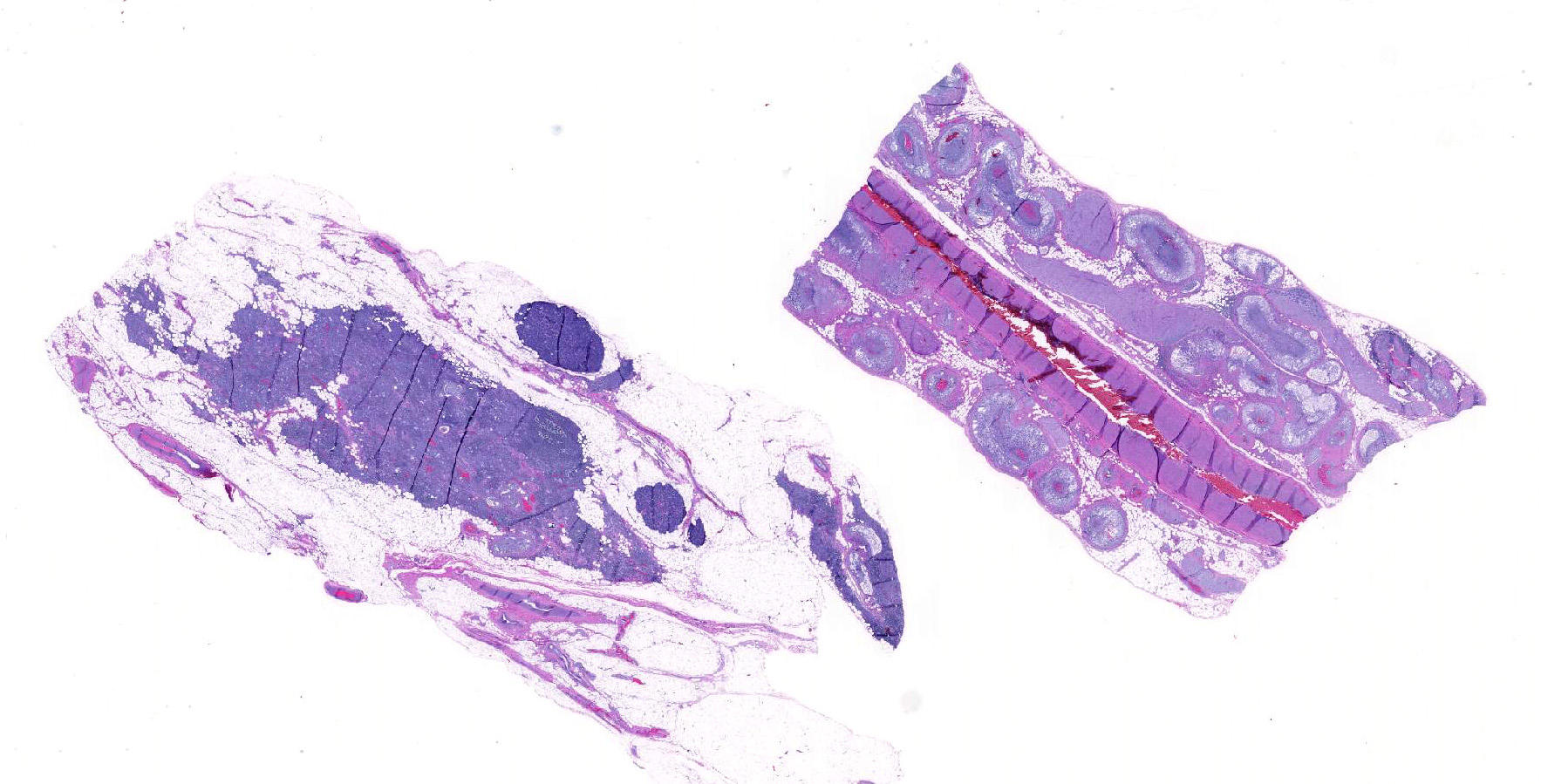
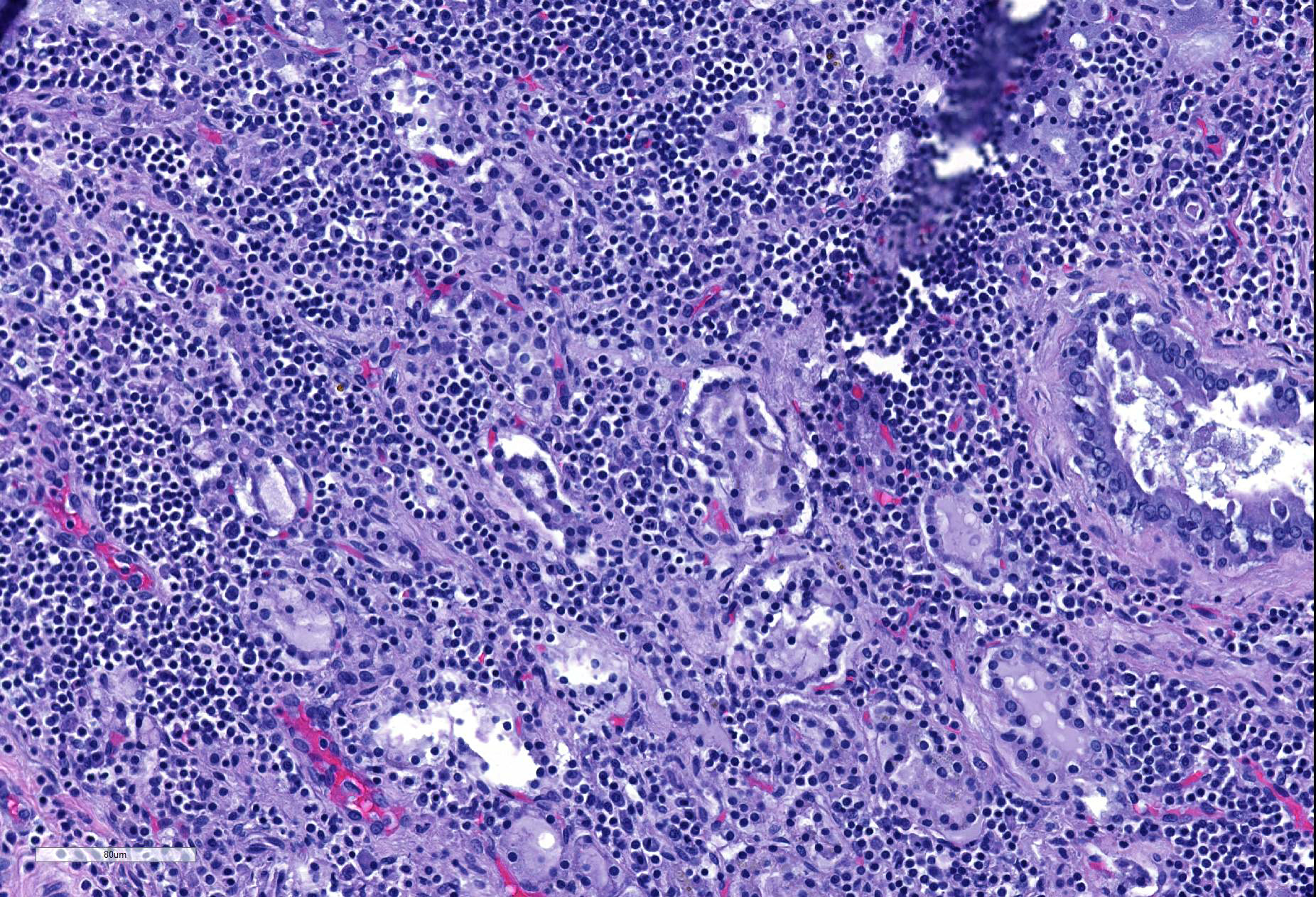
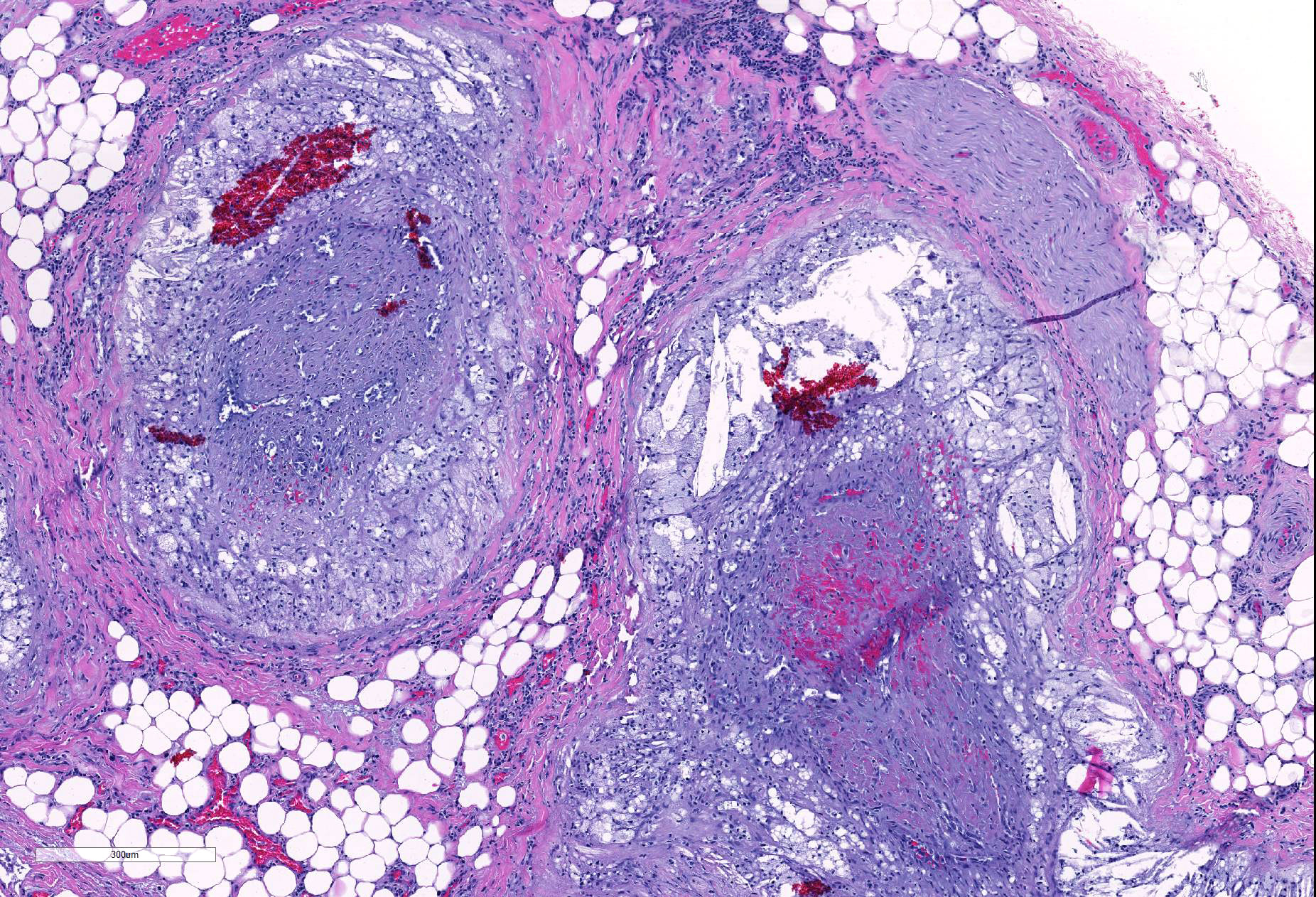
Thyroid: The thyroid glands are small and lack follicles. The follicles are replaced by dense infiltrates of small lymphocytes and plasma cells. The remaining C (parafollicular) cells are prominent. The vessels within and around the gland have foamy macrophages and acicular (cholesterol) clefts replacing and expanding their walls, often resulting in occlusion of the lumen. The parathyroid gland is unremarkable.
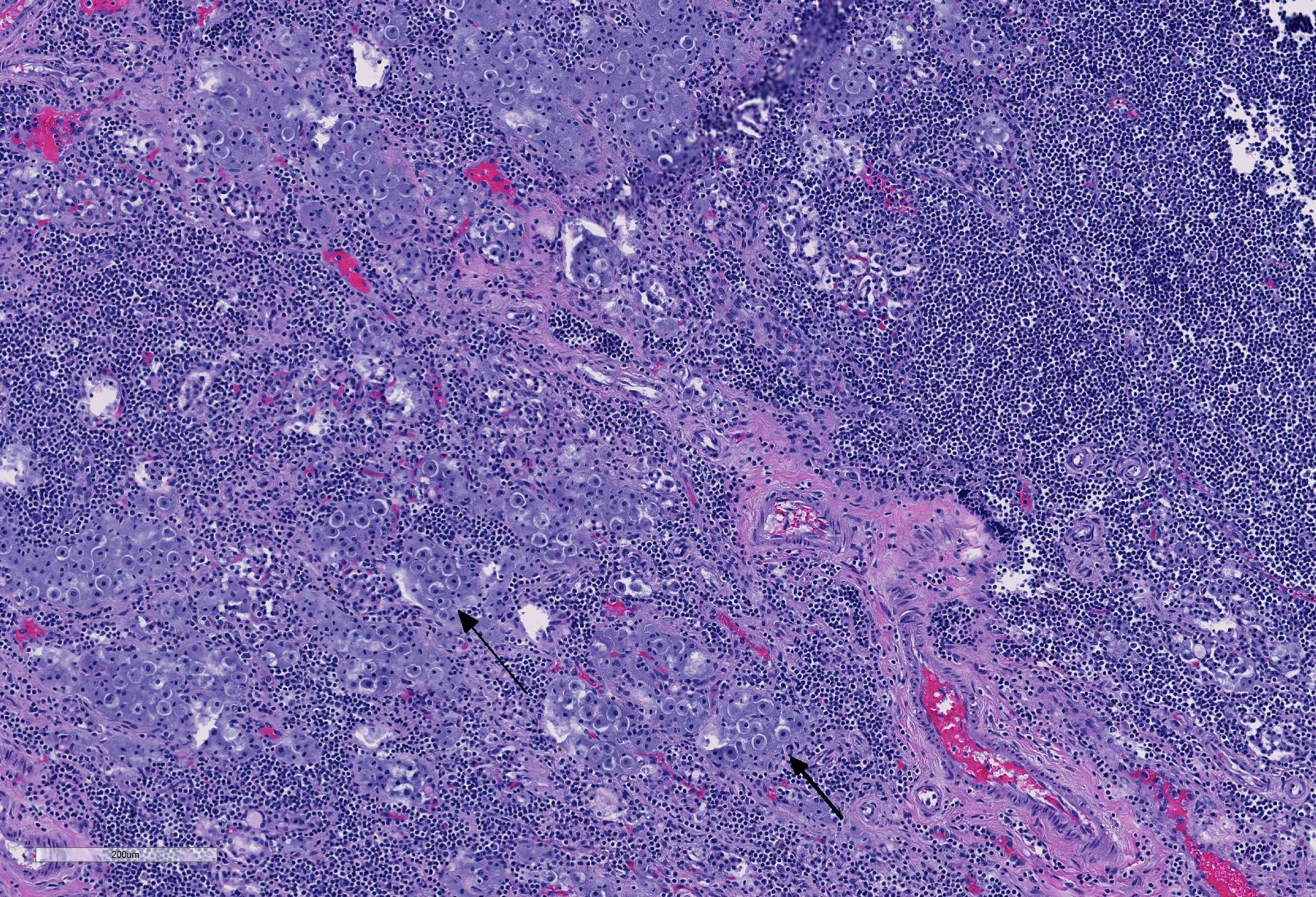
Artery and surrounding vessels: The muscular artery at the center of the section (taken from the hilus of the liver) has mild multifocal expansion of the tunica muscularis by foamy macrophages and small acicular clefts (not present in all sections). The surrounding smaller vessels have severe replacement and expansion of their walls by foamy macrophages and acicular (cholesterol) clefts. The deposits often narrow or occlude the lumens, which occasionally contain thrombi. There is mild lymphoplasmacytic inflammation within the adventitia of the affected vessels.
Contributor’s Morphologic Diagnoses:
Severe chronic diffuse lymphocytic thyroiditis with follicular atrophy
Severe multifocal chronic vascular atherosclerosis with thrombosis
Contributor’s Comment: Lymphocytic thyroiditis in dogs is similar to Hashimoto’s disease of humans. Both are thought to have a polygenic inheritance. Predisposed dog breeds include: boxers, bulldogs, dachshunds, great Danes, Doberman pinschers, golden and Labrador retrievers. Circulating autoantibodies to thyroglobulin are present in affected humans and dogs. Interestingly, the infiltrating lymphocytes and plasma cells are thought to mechanically dislodge the thyroid follicular epithelial cells from their basement membranes resulting in destruction of the follicle.3
The vessel (and nerve) bundle on the submitted slides was taken from the hilus of the liver. The central vessel is presumed to be the hepatic artery (although pretty small for a mastiff). The surrounding more severely affected vessels were presumed to be veins, but veins are reportedly unaffected in canine atherosclerosis.4 Grossly, they resembled lymphatic vessels, but those are also presumably unaffected by atherosclerosis.
This dog had a history of hypothyroidism and had been recently restarted (too late) on his thyroid supplementation in response to his clinical signs. The seizures were likely due to ischemic brain lesions; meningeal and cerebral vessels were occluded by atherosclerosis. Coronary artery atherosclerosis and the resulting myocardial ischemia likely caused the arrhythmia. Externally the findings consistent with hypothyroidism were obesity and tail alopecia.
In summary, this was a case of lymphocytic thyroiditis which led to hypothyroidism which led to hyperlipidemia which led to widespread atherosclerosis which led to cerebral and myocardial ischemia which led to seizures and arrhythmia, respectively.
Contributing Institution:
University of Tennessee College of Veterinary Medicine
Department of Biomedical and Diagnostic Sciences
2407 River Drive, Room A205
Knoxville, TN 37996
https://vetmed.tennessee.edu/departments/Pages/biomedical_diagnostic_sciences.aspx
JPC Diagnosis:
- Thyroid gland: Thyroiditis, lymphoplasmacytic, diffuse, severe with severe follicular atrophy and moderate parafollicular hyperplasia.
- Thyroid gland, adjacent perivascular fibroadipose tissue, arterioles: Atherosclerosis, diffuse, severe with thrombosis and recanalization.
JPC Comment: As discussed above, this case is an excellent example of primary hypothyroidism due to canine lymphocytic thyroiditis (CLT) in the dog. According to various studies, 65-80% of cases are the result of autoimmune disease, with resulting lymphoplasmacytic thyroiditis and destruction of the thyroid gland.2 A number of breeds show a breed predisposition for hypothyroidism, including dobermans, Great Danes, poodles, Irish Setters, miniature and giant schnauzers, boxers, golden retrievers, dachshunds, Shetland Sheepdogs, Pomeranians, Cocker Spaniels and Airedales and Hovawarts.1 Both cellular and humoral mechanisms of immunity are involved in this pathogenesis. Affected animals generally exhibit decreased thyroxine and 75% will demonstrate decreased serum TSH levels. Autoantibodies against thyroglobulin, thyroxine, and triiodothyronine correlate well with lymphocytic thyroid inflammation. In humans, immune complexes containing thyroglobulin have been identified in the basement membrane of thyroid follicles, which may induce NK cell activity and/or complement activation.1
A sensitive assay for thyroglobulin autoantibodies (TGAA) is available and may be positive in animals at a young age, but progression of the disease is variable and cannot be accurately predicted. TGAA positivity has been identified as the first stage of subclinical canine lymphocytic thyroiditis.1 Even when up to 60%-70% of the thyroid has been replaced by lymphocytic inflammation, hypothyroidism may yet be subclinical as a result of overstimulation of remaining follicles by elevated TSH.1 In end stage hypothyroidism, in which almost all thyroid follicles are destroyed (similar to that seen in this case), TGAA may decrease, but TSH, T3, and T4 levels remain abnormal.1 Boxers, Giant Schnauzers, and Hovawarts have been shown to develop CLT with elevated TGAA levels.1
The foamy basophilic to amphophilic cells within the thyroid were discussed during the conference. Some participants thought they represented “oncocytes” (thyroid follicular cells), others believed they were macrophages, while others still thought there were parafollicular c-cells. Participants reviewed a battery of immunohistochemical stains (TTF-1, Iba-1, and synaptophysin and chromogranin-A). The cells in question are diffusely immunoreactive to neuroendocrine markers (chromogranin-A) indicating c-cell origin. It was unclear to the participants whether these cells were hyperplastic, hypertrophic, or simply remnants of normal cells.
References:
- Ferm K, Bjornerfeldt S, Karlsson A, Andersson G, Nacrhtiner R, Hedhammar A. Prevalience of diagnostic characteristics indicating canine autoimmune lymphocytic thyroiditis in giant schnauzer and hovawart dogs. J Small Anim Pract 2009; 50:176-179.
- Mansfield CS, Mooney CT. Lymphocytic-plasmacytic thyroiditis and glomerulonephritis in a boxer. J Small Anim Pract 2006: 47:396-399.
- Rosol TJ, Grone A. Endocrine Glands. In: Maxie MG, ed. Jubb, Kennedy, and Palmer’s Pathology of Domestic Animals. Vol 3, 6th St. Louis Elsevier; 2016:315-319.
- Robinson WF, Robinson NA. Cardiovascular System. In: Maxie MG, ed. Jubb, Kennedy, and Palmer’s Pathology of Domestic Animals. Vol 3, 6th St. Louis Elsevier; 2016:57-59.