Joint Pathology Center
Veterinary Pathology Services
Wednesday Slide Conference
2017-2018
Conference 10
November 29th, 2017
CASE II: JCP-TAMU-1 2017 (JPC 4102431).
Signalment: 1.5-year-old, Domestic shorthair, Felis catus, feline.
History: This 1.5-year-old, castrated-male DSH (Felis catus) was taken to the rDVM on a Tuesday for anorexia, vomiting, and not being as "vocal" as normal. He was treated with an anti-emetic (maropitant and cerenia) and sent home. He hid under the bed all day and had a "seizure." The cat returned to the rDVM on Wednesday where he had a seizure and was hypersalivating. The RDVM did a serum chemistry diagnosing renal failure (Creatinine >20mg/dL (0.3-2.1 mg/dL) and BUN>200 mg/dL (<35 mg/dL)). The cat had elevated serum amylase (2263 U/L (300-1100 U/L)). The cat was referred to TAMU emergency receiving. The cat was dehydrated and quiet but otherwise normal physically. The owner was worried that the cat ate some lilies she had received in Monday. Bloodwork showed severe renal failure. A po or prognosis was given and euthanasia was elected late Tuesday night.
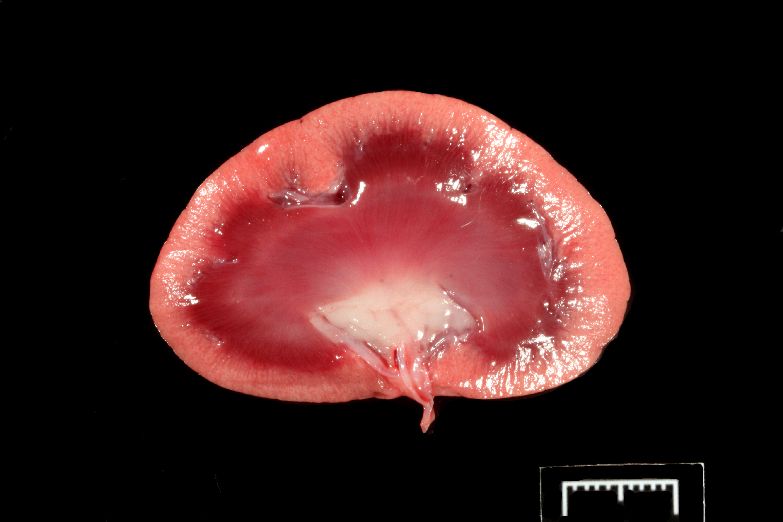
Gross Pathology: A 4.9 kg (10.8 lb), 1.5-year-old, castrated-male, orange tabby Domestic Shorthair cat in good body condition is autopsied on January 19, 2017.
INTEGUMENTARY/SPECIAL SENSES: A 4 cm circumferential band on the left antebrachium and 2x2 cm on the plantar surface of the left crus are shaved. A moderate amount of brown debris (cerumen) is in both external ear canals.
RESPIRATORY: The lungs are diffusely dark red, glistening, and wet, and on section, ooze abundant, red, foamy fluid into the airways (pulmonary edema). A 1.5x2 cm, pale pink, hyperinflated area is at the margins of the cranial lung lobes (emphysema).
CARDIOVASCULAR (Heart weight: 26 g; Right ventricular wall: 1.5 mm; Left ventricular wall: 4 mm), MUSCULOSKELETAL, HEMIC & LYMPHATIC (Spleen weight: 20 g), ENDOCRINE, URINARY (Right kidney weight: 20 g; Left kidney weight: 20 g), GENITAL, DIGESTIVE, LIVER/PANCREAS (Liver weight: 106 g), NERVOUS (Brain weight: 28 g): No significant findings.
Laboratory results:
Blood pressure 120 mmHg (120-180 mmHg)
Severe acidosis pH=7.158 (7.38-7.49))
Hypermagnesimic 0.86 mmol/L (0.38-0.52 mmol/L)
Moderate hyperkalemia 5.09 mmol/L (3.91-4.4 mmol/L),
Azotemia = elevated BUN (250 mg/dL (7-32 mg/dL)) and creatinine 12 mg/dL (0.6-1.9 mg/dL))
Hyperosmotic = osmolarity 377.8 mOsm/kg (291-309 mOsm/kg)
Kidney scraping at necropsy: few birefringent (oxalate presumed) crystals (physiologic normal)
Macroscopically the kidneys were unremarkable.
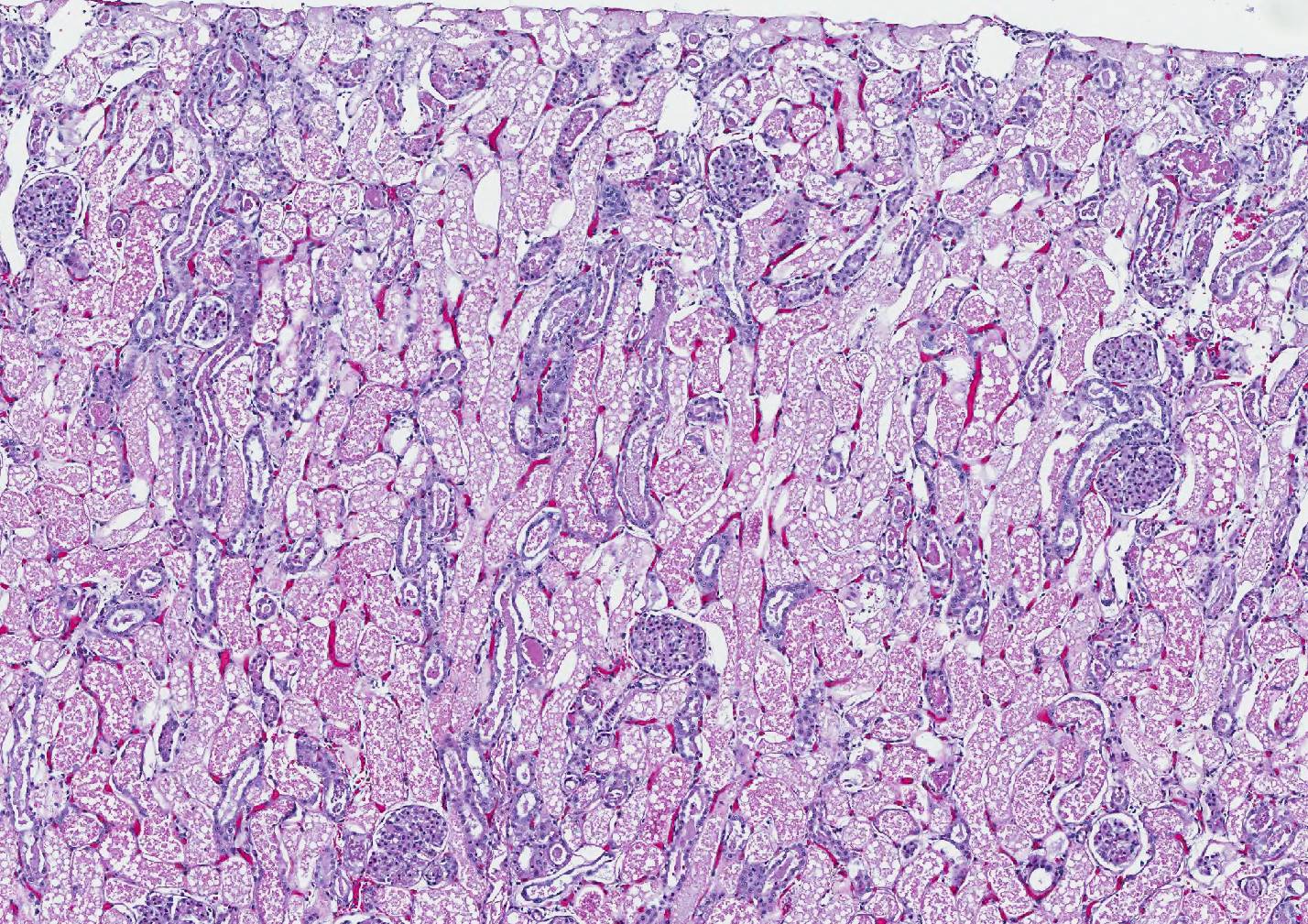
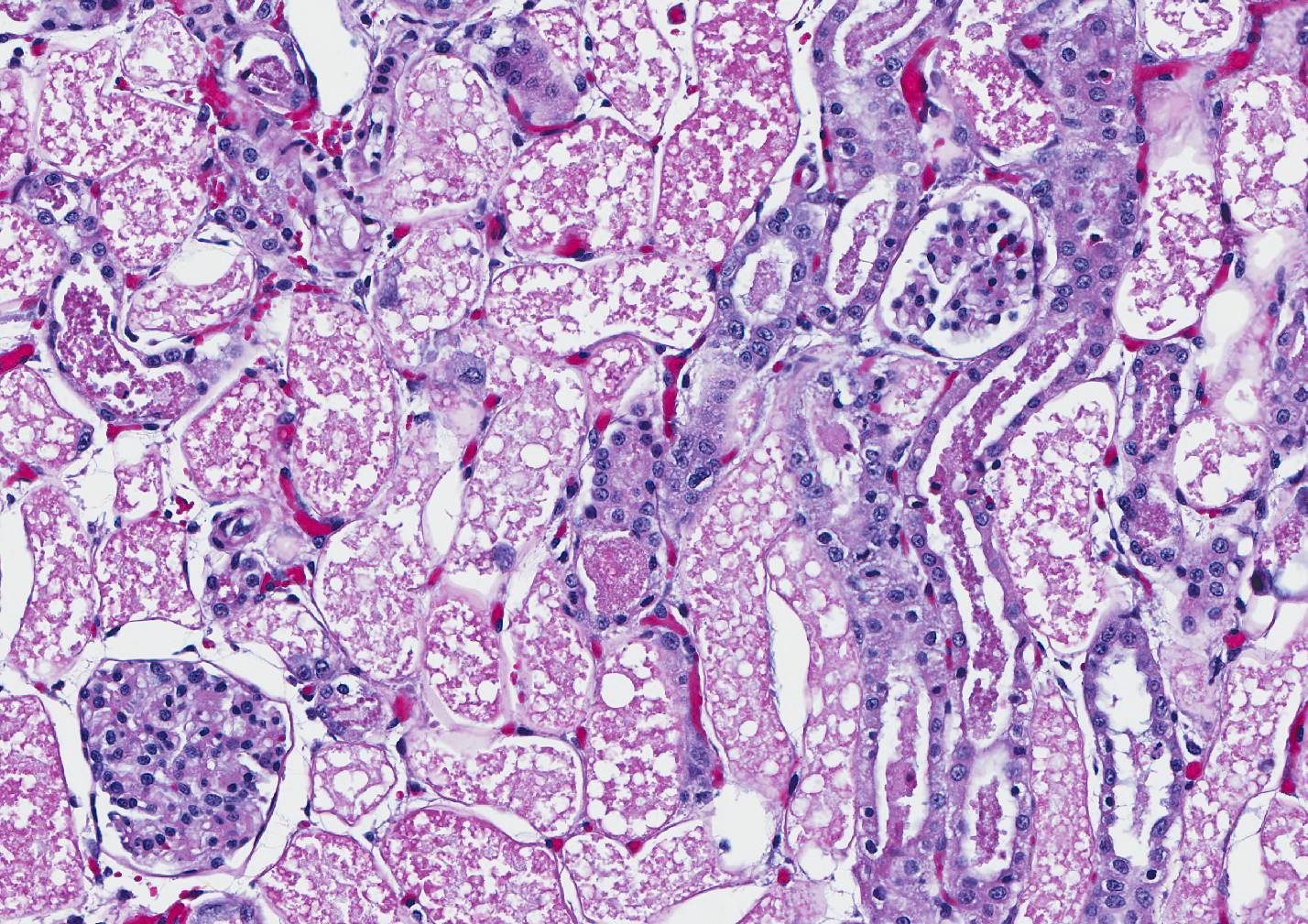
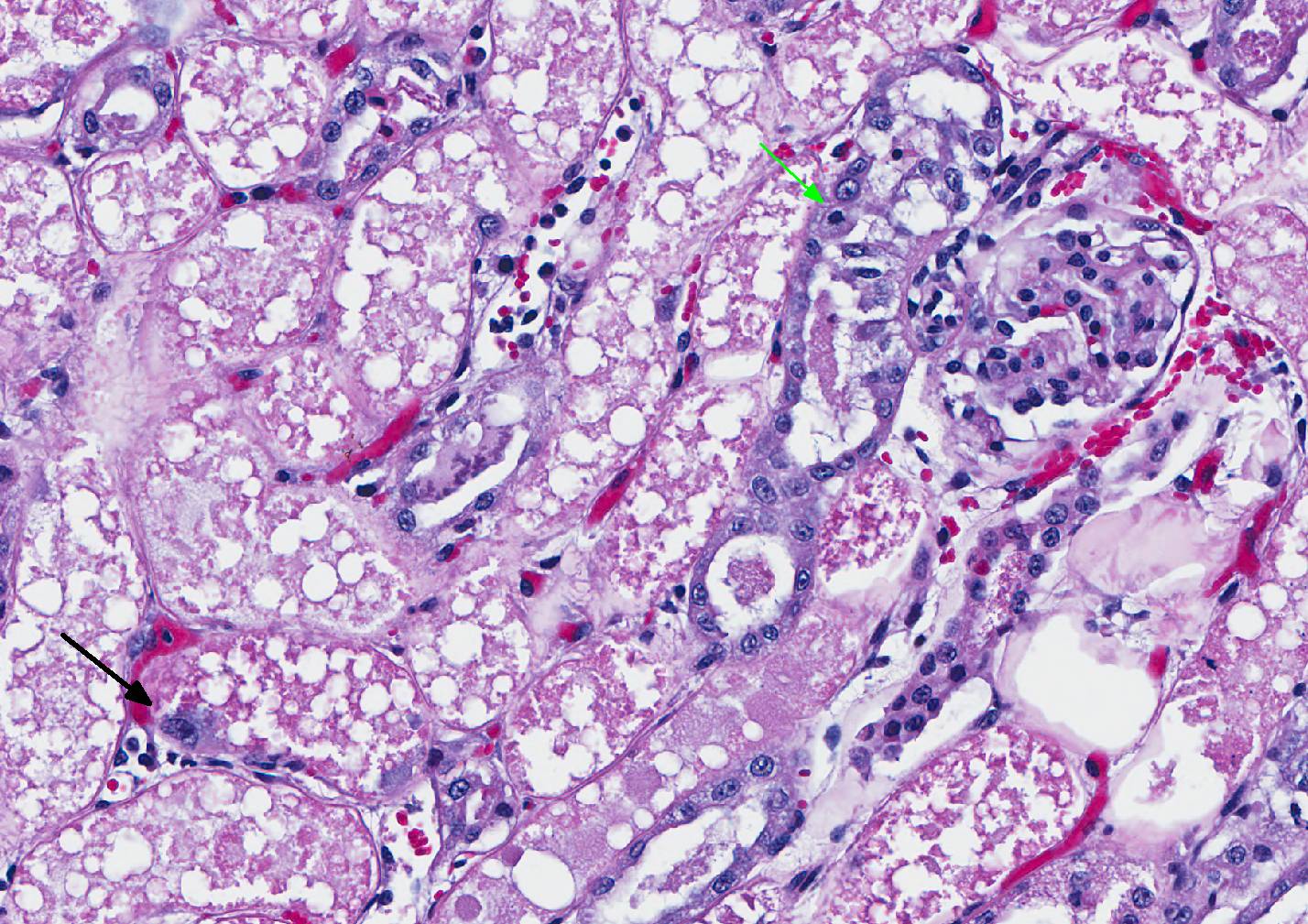
Microscopic Description: Kidney: The section of kidney contains the cortical surface through to the collecting tubules. The proximal tubules are uniformly affected with necrosis and sloughing of tubular cells to fill their lumens. The denuded basement membranes remain intact. Glomeruli are unaffected, and the interstitium is expanded in patches of tubules and around large vessels. Moving toward the corticomedulary junction, tubules begin to have a granular content, and surviving, attenuated tubular cells surround granular cell debris (granular casts). The regenerating tubular cells often have karyomegaly, and the lining cells progressively become more numerous in tubular profiles. Occasionally, deep blue homogeneous orbs are in cell debris (presumed nucleic acid cohesions). In the medullary tubules and collecting ducts the lining cells are normal and tubules contain occasional granular casts. The medulla has a few foci of nephrocalcinosis. Few, presumed, pre-existing foci of interstitial mononuclear inflammation are noted.
Contributor’s Morphologic Diagnosis:
Kidney: Severe subacute proximal tubular necrosis/nephrosis, severe subacute proximal tubular injury; granular tubular casts; tubular regeneration.
Contributor’s Comment: This is a straight forward case of lily intoxication in a cat. 1-3, 6-7, 9 Early onset of vomition, anorexia, hypersalivation, and apathy with rapid progression and later, seizures is usually reported. Unfortunately, as in this case, if early, immediate, rigorous gastric cleansing and fluid diuresis are not instituted, these cases are fatal. The renal lesion is acute proximal tubular necrosis with rupture and sloughing of lining cells leaving tubules full of indistinct cell debris. Ultrastructurally, the cells are characterized by early (<8 hours post exposure) disruption of apical crista, nuclear pyknosis, megamitochondria and some lipid droplet formation.8 The lesions are thought to be the result of hypoxia related to mitochondrial intoxication, and the megamitochondria are the product of mitochondrial fusion. The actual toxins are thought to be several steroidal glycoalkaloids, but are undefined.10 Aqueous extracts of all parts are toxic, and flowers are believed to be more toxic than leaves. Actual experimental cat experiments are limited, but the toxicity curve is steep and different fractions of aqueous extracts, though toxic, are of variable toxicity.
Another lesion seen in cats is pancreatic acinar cell degeneration. 3, 8 It is a subtle lesion consisting of numerous, small vacuoles especially prominent in the basophilic cytoplasmic zone of acinar cells which was seen in this cat. Ultrastructurally, these vacuoles presumably represent lipid vacuoles, again, the result of hypoxia. The increase in amylase reported in some cases, including the one presented, is thought to reflect the acinar cell damage.
Seizuring is reported terminally as in this cat. Although thought to be the result of uremia, the cause of seizuring is felt by some to be more complicated and perhaps involves the effect of the toxin because these seizures are triggered by handling.8 Exposure to lilies inevitably occurs in households with cats that have lilies of many species (growing or delivered as gifts) because cats will seek them out.9 A tragic but fascinating condition.
JPC Diagnosis: Kidney, proximal convoluted tubules: Necrosis, diffuse with regeneration and granular cast formation, Domestic shorthair (Felis catus), feline.
Conference Comment: Several members of the Liliaceae family affect domestic animals, namely, Lilium spp. in cats and Narthecium ossifragum (bog asphodel) in ruminants. Cats and ruminants are affected by ingestion of leaves or flowers of the plants and present with acute onset polyuria, polydipsia, glucouria, proteinuria, isosthenuria, and azotemia.5 The toxic ingredient is unknown, but the acute proximal tubular necrosis that occurs in the kidneys is most likely a result of hypoxia. The most common genera of lily plants, the Easter lily (Lilium longiflorum), affects cats seasonally when plants are brought into their environment; other species: day lily (Hemerocallis spp.), tiger lily (Lilium sp.), Japanese show lily (Lilium hybridum), and rubrum lily (Lilium rubrum) also cause identical renal lesions in cats.4 Additionally, cats have acute pancreatic necrosis and elevated creatinine kinase. Renal tubular epithelial cells have swollen mitochondria, megamitochondria, and accumulation of lipid droplets ultrastructurally.5
The presence of intact basement membranes was demonstrated in the conference with a periodic acid-Schiff with methenamine (PAMS) stain. This stain may be useful in demonstrating tubulorrhexis (induced by ischemia), or its absence (suggestive of acute toxicities). Other differentials for this particular lesion which were briefly discussed included heavy metals, acetaminophen, trimethylprim sulfa, bee or snake venom, various chemotherapeutics, and ethylene glycol. Ethylene glycol could be immediately ruled out in this case because of a lack of intratubular crystal formation.
The blue “orbs” mentioned by the contributor were noticed and admired by conference participants. We agree that they are most likely nucleic acid deposition and are reminiscent of nuclear debris seen in acute tumor lysis syndrome, although their presence in renal tubules is unique.
Contributing Institution:
Texas A&M University
College of Veterinary Medicine and Biomedical Sciences
References:
- Bennett AJ, Reineke EL. Outcome following gastrointestinal tract decontamination and intravenous fluid diuresis in cats with known lily ingestion: 25 cases (2001–2010). J Am Vet Med Assoc. 2013;242:1110–1116.
- Berg RIM, Francey T, Segev G. Resolution of acute kidney injury in a cat after lily (Lilium lancifolium) intoxication. J Vet Intern Med. 2007;21:857–859.
- Brady MA, Janovitz EB. Nephrotoxicosis in a cat following ingestion of Asiatic hybrid lily (Lilium ). J Vet Diagn Invest. 2000;12:566–568.
- Breshears MA, Confer AW. The urinary system. In: Zachary JF, ed. Pathologic Basis of Veterinary Disease. 6th St. Louis, MO: Elsevier; 2017:681.
- Cianciolo RE, Mohr FC. Urinary system. In: Maxie MG, ed. Jubb, Kennedy, and Palmer’s Pathology of Domestic Animals. 2. 6th ed. St. Louis, MO: Elsevier; 2016:428.
- Fitzgerald KT. Lily toxicity in the cat. Topics Comp Anim Med. 2010;25:213-217.
- Langston CE. Acute renal failure caused by lily ingestion in six cats. J Am Vet Med Assoc. 2002;220:49–52.
- Rumbeiha WK, Francis JA, Scott D, et al. A comprehensive study of Easter lily poisoning in cats. J Vet Diagn Invest. 2004;16:527–541.
- Slater MR, Gwaltney-Brant S. Exposure circumstances and outcomes of?48 households with 57 cats exposed to toxic lily species. J Am Anim Hosp Assoc. 2011;47:386–390.
- Uhlig S, Hussain F, Wisløff H. Bioassay-guided fractionation of extracts from Easter lily (Lilium longiflorum) flowers reveals unprecedented structural variability of steroidal glycoalkaloids. 2012;92:42-49.