Signalment:
3-day-old male beef calf, black AngusDiarrhea affecting multiple calves at 3-7 days of age. Calves are unresponsive to treatment and die 1-2 days after onset of clinical signs
Morphologic Diagnosis:
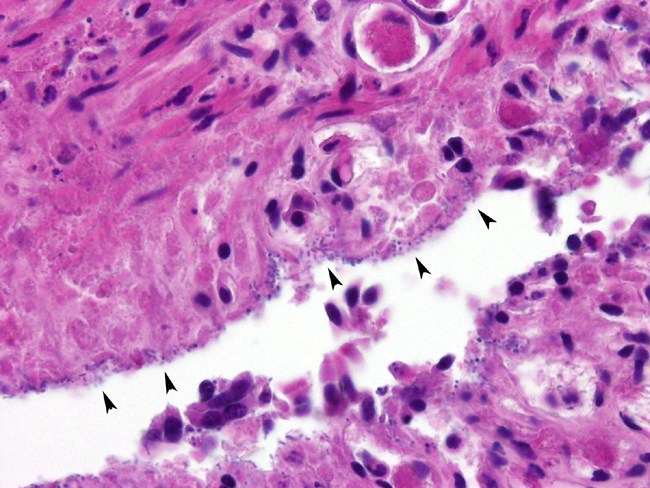
Small Intestine: Enteritis, necrotizing, acute, segmental, marked, with bacilli
Lab Results:
Serum IgG(1) >2000 mg%
E coli K99 negative
Gram stains of intestinal contents reveals moderate bacilli
Clostridium perfringens cultured anaerobically. Cl. perfringens PCR genotyping:
| Alpha | Beta | Epsilon | Iota | Beta2 | Enterotoxin |
| POS | POS | NEG | NEG | NEG | NEG |
Condition:
Clostridium perfringens type C
Contributor Comment:
This is a typical case of neonatal hemorrhagic enterotoxemia (necrotic enteritis) due to
Clostridium perfringens type C, as determined by PCR genotyping. This is a disease of neonatal calves, lambs, foals and piglets
3.Â
Clostridium perfringens types A and C are increasingly common in poultry, due to reduced use of antibiotic growth promoters
4. Clinical signs include hemorrhagic diarrhea, dehydration, anemia and weakness. Although sporadic in occurrence, this disease has a high morbidity and mortality despite treatment. Disease is primarily due to elaboration of cytotoxic beta-toxin. This toxin is readily degraded by trypsin. The trypsin inhibitors in colostrum, effective in facilitating absorption of intact maternal immunoglobulins, also inhibit the degradation of beta-toxin in neonates
5. Death can be due to dehydration and fluid/acid-base derangement or due to secondary gram-negative septicemia/endotoxemia. This case presented with a mild interstitial pneumonia suggestive of bacteremia/endotoxemia and had adequate passive transfer of maternal antibody, both typical ancillary findings. Vaccination for
C. perfringens type C and D is readily available and widely used
JPC Diagnosis:
Small intestine, villi: Necrosis, diffuse, with fibrin thrombi, and myriad mixed bacilli, Angus (
Bos taurus), bovine
Conference Comment:
The five types of
Clostridium perfringens are differentiated by their production of one or more of the four types of antigenic exotoxins.
1 Diagnosis depends on demonstration of the toxin with the presence of hemorrhagic and necrotizing enteritis.
3 Bacterial
colonization (4-1) alone will not produce disease or determine a diagnosis. Disease production is dependent on toxin type and the toxins effect on tissue, either through local toxin inducing necrotizing effects, secretory effects of locally acting enterotoxins, or systemic effects of absorbed (entero)toxins.
1
Alpha toxin is a lecithinase (phospholipase) that damages cell membranes causing necrosis or lysis of erythrocytes, platelets, leukocytes, and endothelial cells. Beta toxin is a trypsin labile, pore forming toxin that causes necrosis, decreases mobility of intestinal villi, and enhances bacterial attachment to the villi. The Epsilon toxin is produced as a prototoxin and activated by enzymatic digestion (i.e, by trypsin in the intestine), and causes necrosis. Iota toxin increases capillary permeability and is also produced as a prototoxin that is activated by proteolytic enzymes.
1
| Clostridium perfringens Types, toxins and diseases |
| Type |
Toxin |
Diseases |
| Alpha |
Beta |
Epsilon |
Iota |
| A | ++ | - | - | - | - Gas gangrene
- Food borne illness humans
- Necrotic enteritis - Chickens
- Gastroenteritis - Ferrets
- Yellow lamb disease - enterotoxemia, western US
- Colitis X in horses - unproven
|
| B | + | ++ | + | - | - Lamb dysentery
- Hemorrhagic enteritis - calves, foals, guinea pigs - UK, S. Africa, Middle East
|
| C | + | ++ | - | - | - Enteroxic hemorrhagic enteritis - neonatal lambs, goats, cattle, pigs
- Struck - Adult sheep, UK
|
| D | + | - | ++ | - | - Overeating disease/pulpy kidney - SHeep, cattle, goats
- Focal symmetric encephalomalacia - Sheep
|
| E | + | - | - | ++ | - Enterotoxemia - calves, lambs, guinea pigs, rabbits
|
| Table adapted from Barker et al, 1993 p.237 & Jones et al, 1997 p. 421 |
Another
Clostridia perfringens toxin identified as +�-�2 has been described in recent literature. Despite its name, +�-�2 toxin is unrelated to the Beta toxin.
1 The gene cpb2 codes for +�-�2-toxin, but not all cpb2 positive strains of
C. perfringens produce the +�-�2 toxin in vitro.
6 It has been implicated in enteric disease in swine and typhlocolitis in horses.
1
References:
1. Brown CC, Baker DC, Barker IK: Alimentary system. In: Jubb, Kennedy, and Palmers Pathology of Domestic Animals, ed. Maxie MG, 5th ed., vol. 2, pp. 213-221. Elsevier Limited, St. Louis, MO, 2007
2. Gelberg HB: Alimentary system. In: Pathologic Basis of Veterinary Disease, eds. McGavin MD, Zachary JF, 4th ed., pp. 358-367. Elsevier, St. Louis, MO, 2007
3. Michelsen PGE: Diseases caused by
Clostridium perfringens toxins (enterotoxemia; yellow lamb disease; lamb dysentery; necrotic enteritis). In: Large Animal Internal Medicine, ed. Smith BP, 3rd ed., Mosby Inc., St. Louis, MO, 2002
4. Van Immerseel F, de Buck J, Pasmans F, Huyghebaert G, Haesebrouck F, Ducatelle R:
Clostridium perfringens in poultry: an emerging threat for animal and public health. Avian Pathol 33:537-549, 2004
5. Radostits OM et al.: Enterotoxemia caused by
Clostridium perfringens types B, C, and E. In: Veterinary Medicine, 9th Ed., pp.770-773. WB Saunders Co., 2000
6. Schotte U, Truyen U, Neubauer H: Significance of +�-�2-toxigenic
Clostridium perfringens infections in animals and their predisposing factors-a review. J Vet Med 51:423-426, 2004