WSC 22-23
Conference 23
Case 3:
Signalment:
2-year-old, female-neutered domestic short hair cat (Felis catus)
History:
The cat was presented in a veterinary practice with acute back pain and mild ataxia after a jump from a cupboard. The clinical examination revealed no specific findings, and the cat was treated with non-steroidal anti-inflammatory drugs (NSAIDs) for a suspected traumatic injury of the vertebral bone and spinal cord. After 2 days without clinical improvement, blood work was performed and displayed mild hypophosphatemia (3.1 mg/dl, reference range: 3.4 – 8.5 mg/dl) and monocytosis (6.6%, reference range: 1 – 3%). The radiological examination showed no abnormalities in the skeleton or spinal cord but a mildly increased interstitial pattern in the craniodorsal lung. The cat was treated further with NSAIDs, antibiotics and vitamin B. Four days after initial presentation, the cat showed mild apathy and severe ataxia with markedly reduced proprioceptive reactions in all four limbs and reduced segmental reflexes in the thoracic limbs. The suspected neuroanatomical localization was the brain or the spinal cord cranially to Th2. No cells were found in the cerebrospinal fluid (CSF). Infection with feline coronavirus, Bornavirus, Toxoplasma gondii and Bartonella henselae within the CSF was excluded via PCR. Computed tomography (CT) of the entire body was performed but showed no abnormalities of the central nervous system. During hospitalization, further progressive clinical decline and irresponsiveness to treatment resulted in lateral recumbency and spontaneous death within 6 days after initial presentation. The cat was subsequently submitted for necropsy.
Gross Pathology:
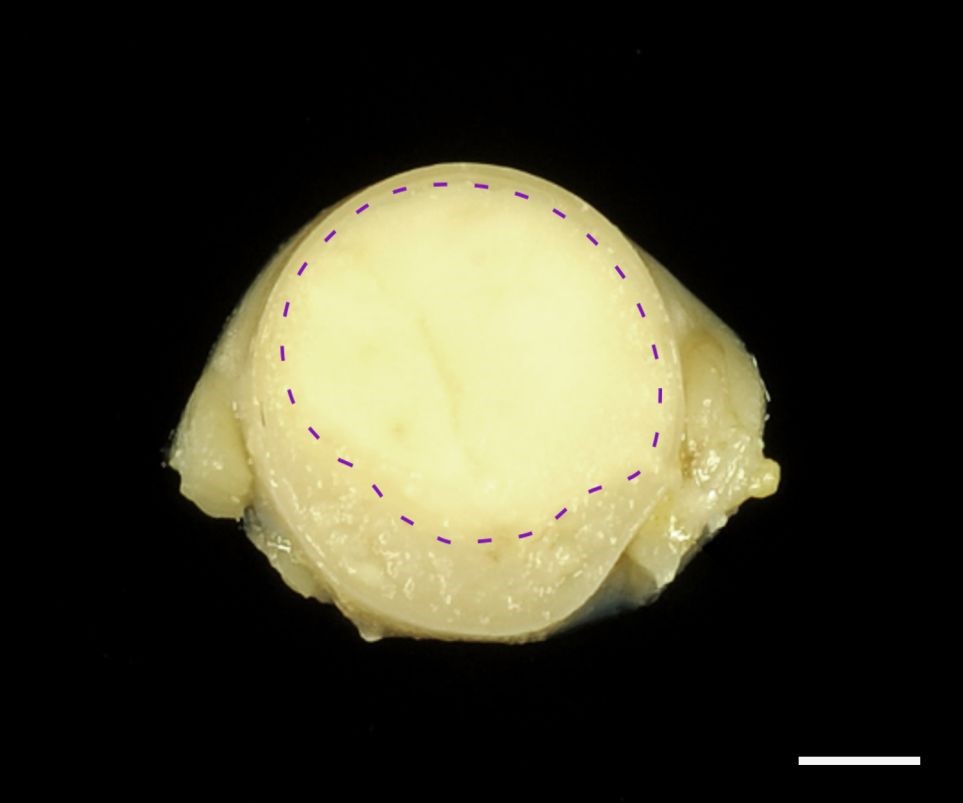
Leptomeninges were diffusely prominent, mostly pronounced within cervical segments with rostral extension to the medulla oblongata. After formalin fixation, cross sections revealed a well demarcated, gray-beige, soft, subdural thickening within the whole circumference of the spinal cord, involving primarily the cervical part, and the medulla oblongata with partial compression of the neuroparenchyma. No intraaxial mass was found in coronal sections of the brain and spinal cord.
Laboratory Results:
The mass was immunostained using the ABC method with commercially available antibodies. Neoplastic cells showed a diffuse, intranuclear expression of oligodendrocyte transcription factor 2 (OLIG2) and doublecortin. Moreover, tumor cells exhibited a diffuse cytoplasmic expression of microtubule-associated protein 2 (MAP2), CNPase and synaptophysin. Some of the neoplastic cells displayed a cytoplasmic vimentin expression. Ki-67 as a proliferation marker protein was detected in more than 50% of the neoplastic cells. Scattered ionized calcium-binding adapter molecule 1 (Iba1)-positive cells and few scattered glial fibrillary acid protein (GFAP)-positive cells were present within the neoplasm (interpreted as reactive macrophages/microglia and astrocytes, respectively). Neoplastic cells lacked immunoreactivity for neurofilament (NF), S100 protein, neuron specific enolase (NSE), myelin basic protein, p75 neurotrophin receptor, neuronal nuclear protein (NeuN), periaxin, pan-cytokeratin, CD3, CD20, CD79a, paired box 5 transcription factor (PAX5) and multiple myeloma oncogene 1 (MUM1).
Microscopic Description:
Spinal cord: Expanding the subarachnoidal space, there is a solid, non-encapsulated, cell-rich, circumferential accumulation of neoplastic cells extending from the arachnoidea to the margins of the spinal cord (Fig. 2). The neoplasm is composed of closely packed, round, mononuclear cells arranged in sheets, accompanied by low amounts of fine fibrovascular stroma (Fig. 3). The medium-sized cells possess variably distinct cell borders and contain low amounts of finely granular eosinophilic cytoplasm. Nuclei measure 10–15 µm in diameter, are centrally to eccentrically located, round to oval and frequently hyperchromatic with one distinct small nucleolus. Multifocally, large necrotic areas with complete loss of cytological details are present (Fig. 4). Tumor cells exhibit mild anisocytosis and –karyosis with a mitotic count of 10 mitoses per 2.37 mm² (with variation throughout the samples). Occasionally, mild hemorrhages are present. The neuroparenchyma adjacent to the tumor multifocally shows compression and marked degenerative changes including spheroid formation and vacuolation of the white and gray matter.
Contributor’s Morphologic Diagnosis:
Spinal cord: Leptomeningeal oligodendrogliomatosis, feline.
Contributor’s Comment:
The presented findings relate to a rare case of primary diffuse leptomeningeal oligodendrogliomatosis, which represents an oligodendroglioma-like tumor with an unusual distribution.
In contrast to other glial tumors, which mostly arise intracranially within the neuroparenchyma and may secondarily infiltrate the leptomeninges, primary diffuse leptomeningeal gliomatosis (PDLG) is defined as a diffuse infiltration of the subarachnoidal space by neoplastic glial cells without evidence of a primary intraaxial tumor.27 Having been described in humans and in dogs before, this entity has recently been reported in an older cat.1,10,21,28 The presented case is the second report of feline PDLG.2
Histologically, oligodendroglial tumors are typically characterized by uniform, densely packed cells with vacuolated or eosinophilic cytoplasm, a round hyperchromatic nucleus and distinct cell borders with variable patterns of cell arrangement. Delayed formalin fixation often causes a perinuclear halo, resulting in a “honeycomb pattern” appearance.25 However, these tumors can vary in their appearance and origin, which requires distinction from other neoplasms (such as lymphomas and neurocytomas) by immunohistochemistry, as performed in the present case. Tumor cells in the present case exhibited an expression of oligodendrocyte transcription factor 2 (OLIG2), doublecortin, microtubule-associated protein 2 (MAP2), CNPase and synaptophysin. Some of the neoplastic cells displayed a cytoplasmic vimentin expression (Fig. 5).
Further differentials in humans and domestic animals for leptomeningeal cell infiltrates include secondary leptomeningeal gliomatosis, ependymoma, pilocytic astrocytoma, or multicentric neoplasia and meningitis of autoimmune or infectious etiology.1,5,11,27 In felines, the most frequently reported extraparenchymatous tumors of the spinal cord are lymphomas and osteosarcomas.14 An infectious disease that needs to be considered in cats for this localization is feline infectious peritonitis (FIP).7,22
To date, the exact origin of PDLG remains unknown. Several authors postulated that PDLG arises from so-called heterotopic glial cell nests, which represent small aggregates of glial cells within the subarachnoid space arising from protrusions of mature glia cells from the neuraxis, but this hypothesis remains controversial.4,5,19 Occasional simultaneous immunopositivity for OLIG2 and neuronal markers like synaptophysin or doublecortin, as also observed in the present case, suggests a histiogenesis from a common progenitor cell.15,16,18
In humans, the incidence of diffuse leptomeningeal oligodendroglioma-like neoplasms is higher in children and young adults when compared to other age groups.20 Several genetic abnormalities have been attributed to oligodendroglial neoplasms in humans including a 1p/19q deletion.26 Concerning domestic animals, brachycephalic dog breeds are predisposed to develop oligodendroglioma with a suspected defect on chromosome 26.23,24 The exclusive representation of brachycephalic dogs (4 boxer dogs, 1 Staffordshire bull terrier, 1 Cane Corso) in published cases of canine diffuse leptomeningeal gliomatosis may propose a similar breed disposition to PDLG.1,8,10,12 However, further case data need to be obtained to confirm this assumption. No specific genetic alterations have been determined so far for PDLG in domestic animals.
Intravital diagnosis of PDLG, which is predominantly based on MRI findings and exclusion of other diseases, is challenging due to relatively unspecific clinical and CSF findings and requires histopathological confirmation.1,5,6,8,10,12,27,28 In most cases, final diagnosis is made at necropsy due to the rapid progression and poor prognosis of the tumor.5
Contributing Institution:
Department of Pathology,
University of Veterinary Medicine,
Hannover,
Buenteweg 17,
30559 Hannover, Germany.
http://www.tiho-hannover.de/kliniken-institute/institute/institut-fuer-pathologie/
JPC Diagnosis:
Leptomeninges, spinal cord: Oligodendrogliomatosis.
JPC Comment:
The moderator and conference participants had spirited discussion over the morphologic diagnosis in this case. As the contributor mentions, it is impossible to determine whether the oligodendrogliomatosis is a primary lesion, or if it arose secondary to a small primary tumor not in section. Due to this uncertainty, some participants favored a broader diagnosis of oligodendroglioma; however, most felt that the term oligodendrogliomatosis would provide valuable information for the clinicians, as a focal oligodendroglioma would not be consistent with the neurologic signs, advanced imaging patterns (MRI with contrast), and gross lesions produced by a diffuse leptomeningeal lesion.
In this section, there is a small focus of fibrosis within the meninges, and some participants considered a second morphologic diagnosis of fibroma. The moderator explained that focal fibrosis within the meninges and in the nerve sheath is a common aging change in geriatric animals and is not considered abnormal in this case.
In a 2020 Vet Pathol article, Kauer et al described leptomeningeal olgodendrogliomatosis in a 4.5 year old cow which died after progressive neurologic signs, including ataxia, circling, and tremors.9 Grossly, the leptomeninges spanning the cerebellum, ventral occipital lobe, and first cervical spinal cord segment were expanded by a gelatinous, tan to gray mass that protruded into the third and fourth ventricles and extended into the thalamus.9 Histologically, the neoplastic cells were uniformly round and hyperchromatic, arranged in sheets, nests, and cords, and surrounded by a myxoid matrix.9 There were multifocal microcysts filled with mucin. Multifocal areas of necrosis, microvascular proliferation, and a high mitotic rate were indicative of malignancy.9 The vast majority of tumor cells had strong nuclear immunoreactivity for Olig-2.9 These features were consistent with a diffuse high-grade leptomeningeal oligodendrogliomatosis.9 While this is the first documented bovine case of diffuse leptomeningeal oligodendrogliomatosis, two previously documented cases of oligodendrogliomas in cows also featured this diffuse leptomeningeal growth without identification of a primary neoplasm. The authors suggest that these prior cases may also be instances of diffuse leptomeningeal oligodendrogliomatosis.9
Two other rare proliferative lesions of the leptomeninges have recently been reported in cats: angiocentric astrocytoma and meningiomatosis.3,17 In a 2019 Vet Pathol article, Rissi et. al described the first veterinary case of angiocentric astrocytoma in a 15 year old cat with seizures refractory to medical therapy.17 On necropsy examination, the leptomeninges surrounding the olfactory bulbs were swollen and firm with multifocal hemorrhage.17 Histologically, blood vessels within the leptomeninges of the olfactory bulb and extending caudally to the thalamus were surrounded by polygonal to elongate, sometimes palisading neoplastic cells.17 No primary neoplasm was identified. On IHC, these cells had strong reactivity for GFAP, S100, and vimentin.17 The histologic morphology, IHC staining, and ultrastructure features of this case were all consistent with a diagnosis of astrocytoma, and this case bears many similarities to human angiocentric astrocytoma, a rare entity in children and young adults.17
The first documented case of meningioangiomatosis in a cat was recently reported by Corbett et al.3 Previously, this rare entity has been described in humans and dogs. Corbett’s report details a 13 year old cat with history of acute behavioral changes, open mouth breathing, and facial twitching that progressed to generalized seizures.3 The animal died despite 5 days of hospitalization, and on necropsy, a unilateral hemorrhagic plaque expanded the meninges over the right pyriform, temporal, and ventral aspect of the occipital lobes and extended into the subjacent cerebral cortex.3 Histologically, the leptomeninges were thickened by proliferations of vimentin-positive spindle cells streaming and whirling around blood vessels.3 The histomorphology and IHC profile were consistent with the cases of meningioangiomatosis documented in humans and dogs.3
References:
- Canal S, Bernardini M, Pavone S, et al. Primary diffuse leptomeningeal gliomatosis in 2 dogs. Can Vet J. 2013;54: 1075–1079.
- Chludzinski E, Puff C, Weber J, et al. Case Report: Primary diffuse leptomeningeal oligodendrogliomatosis in a young adult cat. Front Vet Sci. 2021;8: 795126.
- Corbett MP, Kopec BL, Kent M, Rissi DR. Encephalic meningioangiomatosis in a cat. J Vet Diagn Invest. 2022; 34(5): 889-893.
- Cooper IS, Kernohan JW. Heterotopic glial nests in the subarachnoid space; histopathologic characteristics, mode of origin and relation to meningeal gliomas. J Neuropathol Exp Neurol. 1951;10: 16–29.
- Debono B, Derrey S, Rabehenoina C, et al. Primary diffuse multinodular leptomeningeal gliomatosis: case report and review of the literature. Surg Neurol. 2006;65: 273–282; discussion 282.
- Dietrich PY, Aapro MS, Rieder A, et al. Primary diffuse leptomeningeal gliomatosis (PDLG): a neoplastic cause of chronic meningitis. J Neurooncol. 1993;15: 275–283.
- Fondevila D, Vilafranca M, Pumarola M. Primary central nervous system T-cell lymphoma in a cat. Vet Pathol. 1998;35: 550–553.
- Giron C, Paquette D, Culang D, et al. Diffuse meningeal oligodendrogliomatosis characterized by spinal intra-parenchymal nodules on magnetic resonance imaging in a dog. Can Vet J. 2020;61: 1312–1318.
- Kauer RV, Bagatella S, Oevermann A. Diffuse Leptomeningeal Oligodendrogliomatosis in a Cow. Vet Pathol. 2020; 57(2): 253-257.
- Kovi RC, Wünschmann A, Armién AG, et al. Spinal meningeal oligodendrogliomatosis in two boxer dogs. Vet Pathol. 2013;50: 761–764.
- Lee JK, Ko HC, Choi JG, et al. A Case of diffuse leptomeningeal glioneuronal tumor misdiagnosed as chronic tuberculous meningitis without brain biopsy. Case Rep Neurol Med. 2018;2018: 1391943.
- Lobacz MA, Serra F, Hammond G, et al. Imaging diagnosis – magnetic resonance imaging of diffuse leptomeningeal oligodendrogliomatosis in a dog with “dural tail sign”. Vet Radiol Ultrasound. 2018;59: E1–e6.
- Louis DN, Perry A, Reifenberger G, et al. The 2016 World Health Organization classification of tumors of the central nervous system: a summary. Acta Neuropathol. 2016;131: 803–820.
- Marioni-Henry K, Van Winkle TJ, Smith SH, et al. Tumors affecting the spinal cord of cats: 85 cases (1980-2005). J Am Vet Med Ass. 2008;232: 237–243.
- Perry A, Scheithauer BW, Macaulay RJ, et al. Oligodendrogliomas with neurocytic differentiation. A report of 4 cases with diagnostic and histogenetic implications. J Neuropathol Exp Neurol. 2002;61: 947–955.
- Rissi DR, Levine JM, Eden KB, et al. Cerebral oligodendroglioma mimicking intraventricular neoplasia in three dogs. J Vet Diagn Invest. 2015;27: 396-400.
- Rissi DR, McHale BJ, Armien AG. Angiocentric astrocytoma in a cat. J Vet Diagn Invest. 2019; 31(40: 576-580.
- Rissi DR, Miller AD. Feline glioma: a retrospective study and review of the literature. J Feline Med Surg. 2017;19: 1307–1314.
- Riva M, Bacigaluppi S, Galli C, Citterio A, Collice M. Primary leptomeningeal gliomatosis: case report and review of the literature. Neurol Sci. 2005;26: 129–134.
- Rodriguez FJ, Perry A, Rosenblum MK, et al. Disseminated oligodendroglial-like leptomeningeal tumor of childhood: a distinctive clinicopathologic entity. Acta Neuropathol. 2012;124: 627–641.
- Roussy G, Cornil L, Leroux R. Tumeur meningee a type glial. vol. 30. Paris: Rev. Neurologique.1923:30: 294–298.
- Shrader S, Lai S, Cline K, et al. Gliomatosis cerebri in the brain of a cat. Vet Sci. 2016;3 (3): 13. doi: 10.3390/vetsci3030013.
- Snyder JM, Shofer FS, Van Winkle TJ, et al. Canine intracranial primary neoplasia: 173 cases (1986-2003). J Vet Intern Med. 2006;20: 669–675.
- Truvé K, Dickinson P, Xiong A, et al. Utilizing the dog genome in the search for novel candidate genes involved in glioma development - genome wide association mapping followed by targeted massive parallel sequencing identifies a strongly associated locus. PLoS Genet. 2016;12 (5): e1006000. doi: 10.1371/journal.pgen.1006000.
- Vandevelde M, Higgins R, Oevermann A. Neoplasia. In: Veterinary Neuropathology: Essentials of Theory and Practice. Ames, IA, USA: Wiley-Blackwell; 2012:137–139.
- Wesseling P, van den Bent M, Perry A. Oligodendroglioma: pathology, molecular mechanisms and markers. Acta Neuropathol. 2015;129: 809–827.
- Yomo S, Tada T, Hirayama S, et al. A case report and review of the literature. J Neurooncol. 2007;81: 209–216.
- Zoll WM, Miller AD, Bandt C, et al. Primary leptomeningeal gliomatosis in a domestic shorthaired cat. J Vet Diagn Invest. 2019;31: 94–97.