Joint Pathology Center
Veterinary Pathology Services
Wednesday Slide Conference
2018-2019
Conference 7
October 17, 2018
CASE I: UW Case 1 (JPC 4084541-00).
Signalment: 15-year-old female spayed Himalayan feline, Felis catus
History: The patient presented to the University of Wisconsin–Madison Veterinary Medical Teaching Hospital and was diagnosed with a blind left eye (OS), granulomatous infiltrate in the anterior chamber, posterior chamber and vitreous (OS) and bilateral corneal ulcers. The left eye was enucleated, formalin-fixed and submitted for histopathology.
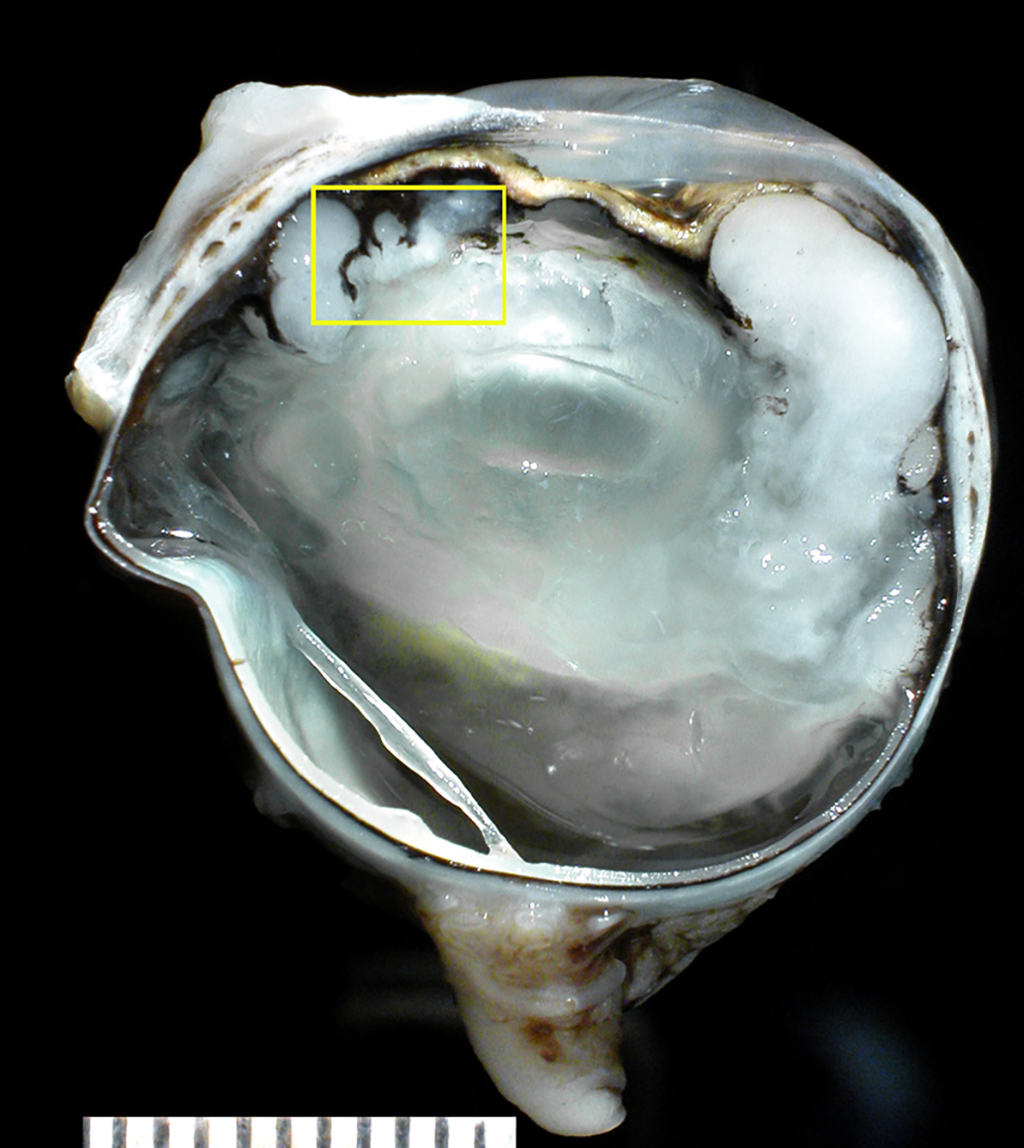
Gross Pathology: The formalin-fixed left eye was section at the dorsoventral plane. There was a white homogeneous tissue carpeting the surfaces of the iris and ciliary body and extending into the posterior chamber and anterior vitreous, cradling the lens.
Laboratory results: Thoracic radiographic studies and abdominal ultrasound were within normal limits.
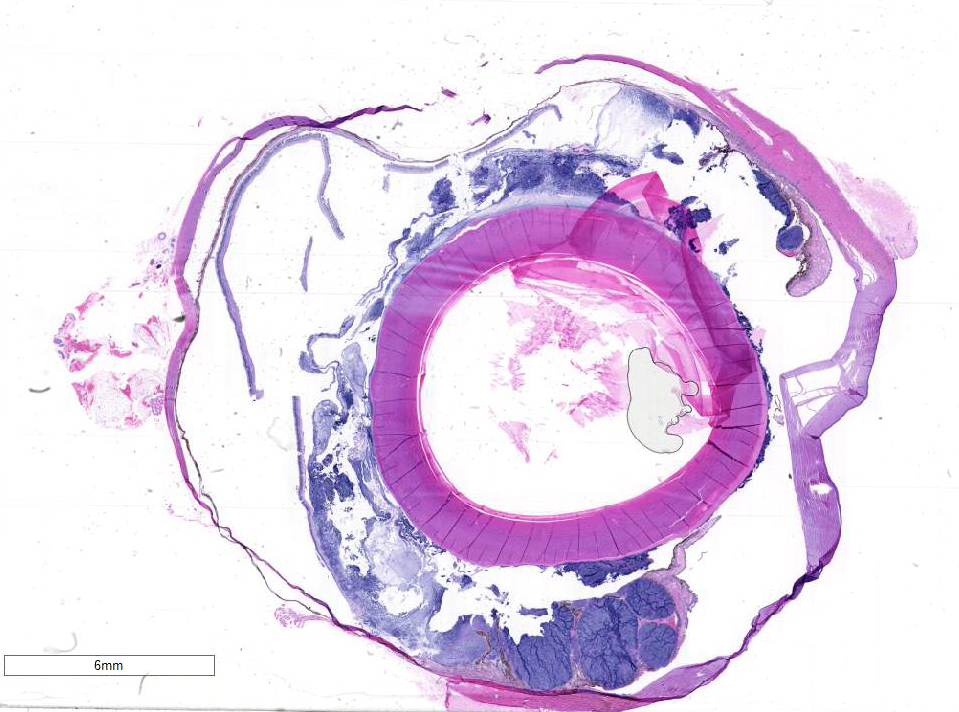
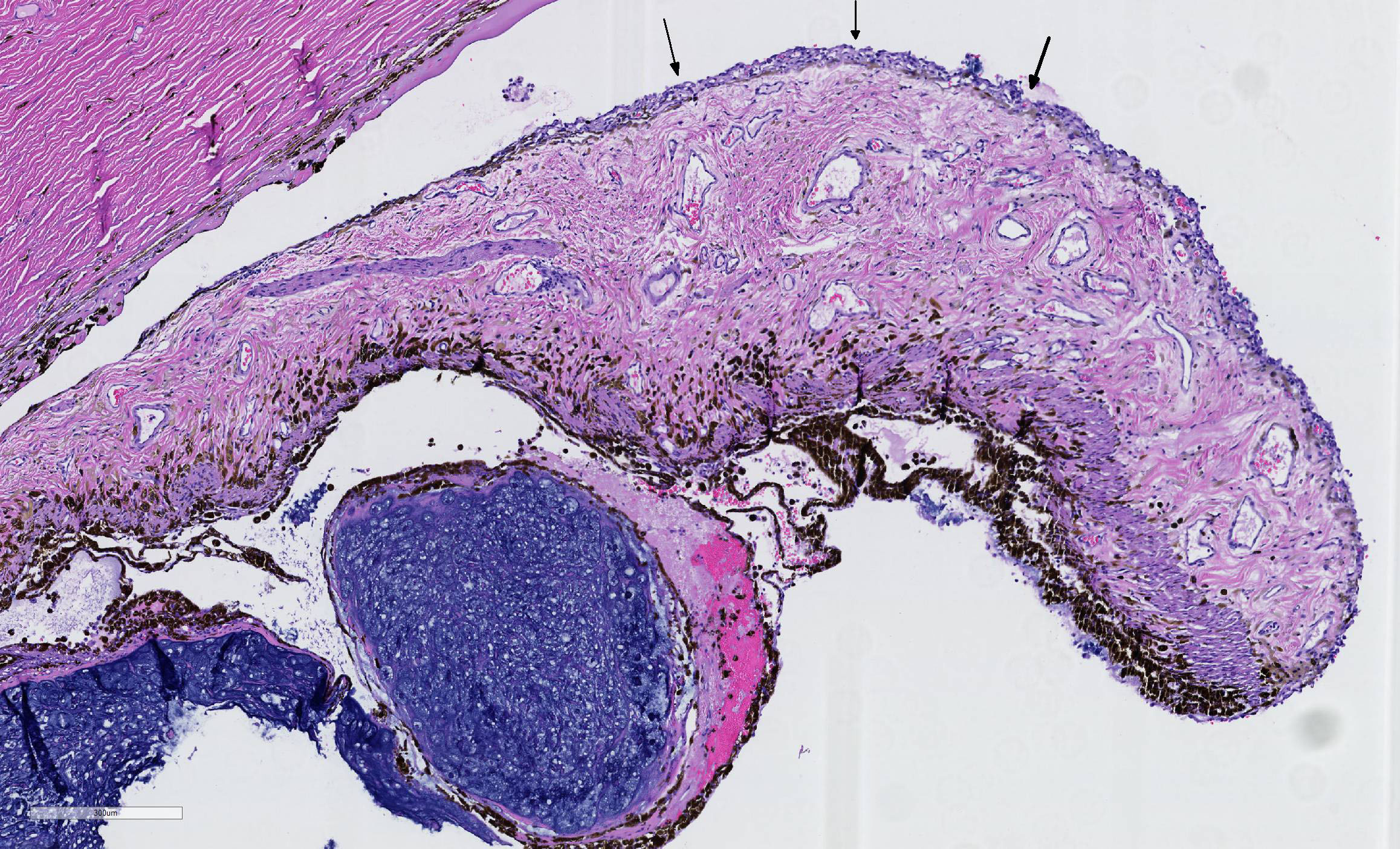
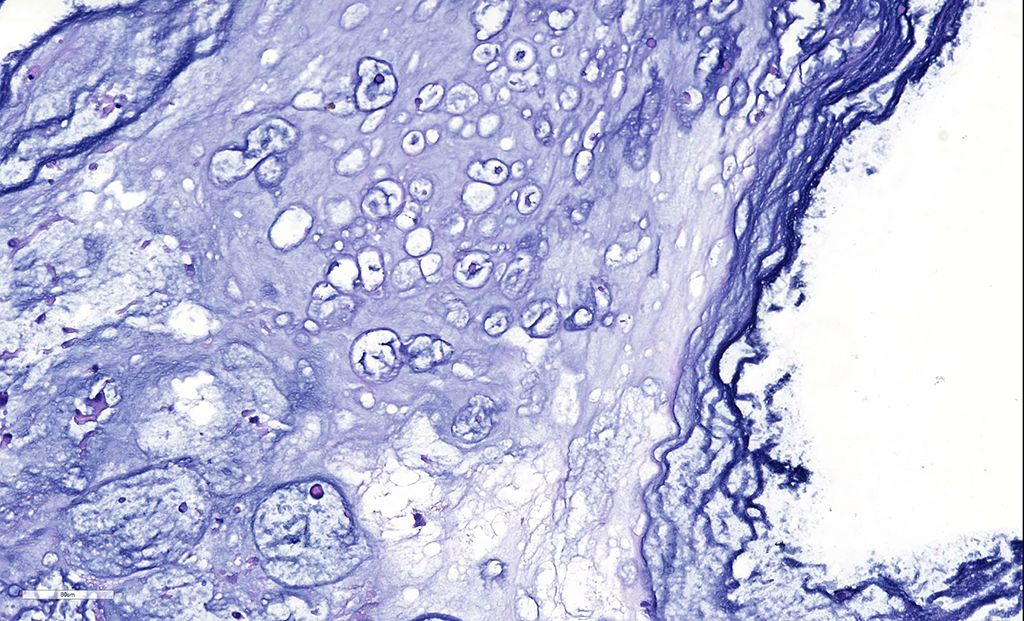
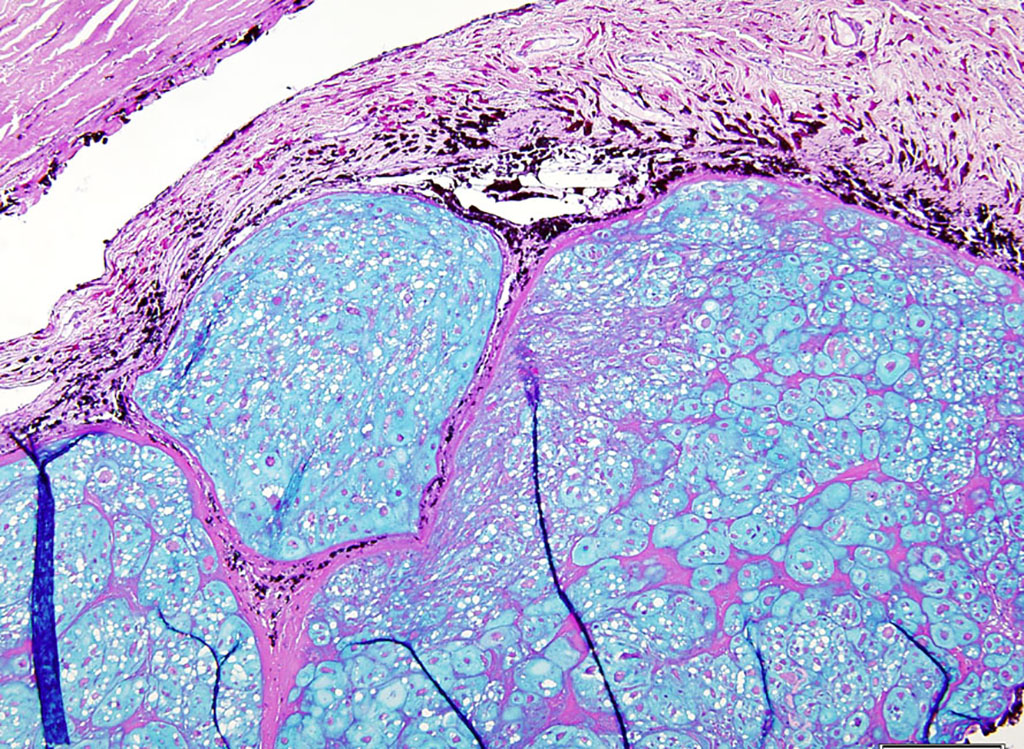
Microscopic Description: There is a poorly delineated, moderately cellular and hypereosinophilic neoplastic mass carpeting the posterior iris and ciliary body surfaces, infiltrating and expanding the inferior iris leaflet stroma and extending into the anterior chamber, posterior chamber and anterior vitreous, surrounding the lens capsule. The mass is composed of haphazardly arranged plump neoplastic cells surrounded by dense, highly basophilic chondromatous matrix. Neoplastic cells are individualized or aggregated in lacunae within the matrix and have a moderate amount of granular eosinophilic to basophilic cytoplasm. Nuclei are oval, have 1-2 magenta nucleoli and finely stippled chromatin. The mitotic rate averages less than one per 10 HPF. There are focally extensive areas of necrosis comprising approximately 20% of the mass. There is a fibrovascular membrane carpeting the anterior surface of the iris (preiridal fibrovascular membrane). There is moderate liquefaction of the cortical lens fibers with accumulation of round and lightly eosinophilic degenerated fibers (Morgagnian globules) and migration of the lens epithelial cells over the inner aspect of the posterior lens capsule. The retina is artifactually detached. The inner retina is devoid of ganglion cells and that are diminished numbers of nuclei in the inner nuclear layer. The optic nerve is markedly gliotic and atrophied (optic nerve not present in all sections).
Contributor’s Morphologic Diagnoses:
Left eye:
- Chondrosarcoma, primary.
- Lens, circumferential and moderate cortical lens fiber degeneration and posterior lens epithelial migration (mature cortical cataract).
- Retina, marked and diffuse inner retinal atrophy (secondary chronic glaucoma).
- Optic nerve, marked and diffuse optic nerve gliosis and atrophy (secondary chronic glaucoma).
Contributor’s Comment: Chondrosarcomas are uncommon malignant neoplasms with predominating cartilaginous matrix that account for the second most common primary skeletal tumor after osteosarcoma in both veterinary and human medicine.5 The average age of cats affected by chondrosarcomas is 9.6 years, and there is a slight male predilection for the development of these tumors.5 Extraskeletal chondrosarcomas, and visceral ones in particular, are rare tumors in dogs, cats and people.5,7 In a case series of 67 cats with chondrosarcomas, 47 were tumors of skeletal origin and 20 presented in subcutaneous sites, several of which were thought to be vaccine-site sarcomas.5 Intraocular chondrosarcoma is reported in two dogs as a primary11 or metastatic8 neoplasm. Metastatic intraocular chondrosarcoma was also reported in one human patient.6 In 1959, a single account was published describing an intraocular chondrosarcoma in a cat presenting with multiple intraocular tumors.2 Recently, we reported 4 cases of presumed primary intraocular chondrosarcoma in cats (including the present case).2 The mean age of the animals was 12.5 (range 9-16) and the tumors presented unilaterally as coalescing, poorly demarcated, white, friable masses filling the vitreous and intraocular chambers. One tumor presented as a solitary, well-demarcated, tan mass involving the iris and ciliary body. All four neoplasms were composed of haphazardly arranged plump neoplastic spindle cells surrounded by irregular islands and thick trabeculae of abundant, variably basophilic and Alcian-blue-positive chondromatous matrix. No other tumors or skeletal lesions were identified in these four cats that could suggest a metastatic tumor to the eye. Two of the four cats diagnosed with primary ocular chondrosarcoma are still alive and healthy 2.5 years and 5 years following enucleation. One cat died 6 months after enucleation due to chronic kidney disease and diabetes and although no necropsy was performed, imaging done in the follow-up visits still did not revealed other masses. The last cat was lost to follow-up.
Due to the distribution of the neoplastic tissue on the eye (posterior chamber and anterior vitreous, surrounding the lens) and because of the chondromatous nature of the mass a post-traumatic sarcoma (chondrosarcoma) is a possible differential diagnosis. Feline post-traumatic sarcomas (FPTS) are malignant, intraocular neoplasms that are usually associated with trauma that can be evidenced from the clinical history and/or histologic findings (e.g. lens capsule rupture, retinal detachment, and corneal perforation)3,4. We ruled out the diagnosis of FPTS in the present case based on the absence of a history of trauma and/or histologic features of trauma, especially lens capsule rupture, which appears to be a major step on the development of the post-traumatic sarcoma, allowing the lens epithelial cells to gain access to the extra-capsular space, proliferate over the ocular tissues and eventually become neoplastic.1,11
Cats, similar to all mammals, do not have cartilage or bone within their globes and, therefore, the tissue of origin of the primary ocular chondrosarcoma is unclear. It is likely that primary intraocular chondrosarcomas arise from ocular multipotent mesenchymal stem cells or cancer stem cells..9 In human eyes, multipotent mesenchymal stem cells have been derived from the trabecular meshwork.9 The trabecular meshwork could be a likely origin of the tumors seen in these cases, all of which showed extensive involvement in the vicinity of the iris, ciliary body and ciliary cleft.
Contributing Institution:
Comparative Ocular Pathology Laboratory of Wisconsin - COPLOW
School of Veterinary Medicine
Department of Pathobiological Sciences
University of Wisconsin – Madison
http://www.vetmed.wisc.edu/departments/pathobiological-sciences/
http://uwveterinarycare.wisc.edu/
http://uwveterinarycare.wisc.edu/support-services/laboratory/anatomic-pathology/
JPC Diagnosis: Eye, iris and ciliary body: Chondrosarcoma.
JPC Comment: The moderator, who was also the contributor of this case, has provided an excellent review of this uncommon lesion, as well as the primary differential diagnosis and secondary changes in the section.
In bone and beyond, a diagnosis of chondrosarcoma may be complicated by a number of factors, not the least of which is small sampling. Both the production of osteoid (which changes a diagnosis of chondrosarcoma to a diagnosis of osteosarcoma) as well as malignant features of neoplastic chondrocytes may be lacking in small samples and present in more liberal ones.10 Due to their poorly vascularized nature, many sarcomas contain extensive areas of necrosis and/or mineralization, and these areas should be avoided when evaluating the malignant features of a potential chondrosarcoma.10 When evaluating for potential malignancy, the most obviously atypical area of the tumor deserves primary focus. Malignant features include: more than an occasional bi-nucleated cell (as seen in this case), numerous cells with prominent nuclei, and mitotic figures (which may be extremely rare in more well differentiated malignancies).10 Chondrosarcomas often contain cellular populations of great morphological variety, including small cells with hyperchromatic nuclei resembling the mesenchymal precursors of cartilage,10 which were seen in this section as well. Intercellular matrix may range in color from pink to blue, as well as the amount present, and mucinous or myxoid matrix may predominate.
In conference, the moderator discussed three potential diagnoses for this case of an obvious chondromatous neoplasm within the globe: a) a primary ocular chondrosarcoma, b) a chondrosarcoma metastatic to the globe, and c) a post-traumatic sarcoma. The moderator noted the absence of any variation in the morphology of the neoplasm, particularly that of in the absence of a spindle cell or osseous component, which would be unusual for a post-traumatic sarcoma, which often has a mix of morphologies. In addition, post traumatic sarcomas are often associated with a tear in the lenticular capsule, which is absent in this specimen.
He also noted that the pattern of “carpeting” of posterior aspect of the ciliary body, as well as the lack of infiltration into this tissue suggests a metastatic process. Other characteristics of ocular metastasis is the formation of a well-demarcated mass within the globe. Presence of neoplastic emboli within the vessels of the choroid or uvea may or may be seen with metastatic tumors. The presence of a primary process elsewhere in the body is ultimately a major consideration, and this was a case submitted by the moderator, who was were unable to identify a primary process elsewhere in the body. COPLOW currently has a total of 7 similar lesions in cats in their database – 5/7 were alive after 2.5 years, the remaining two died of unrelated causes.
Another discussion centered upon whether the retina was artifactually or truly detached. For most of its circumference, photoreceptors remained attached to the RPE, suggesting artifactual detachment. However, there are focal areas in of RPE hypertrophy (tombstoning) as well scattered along the retina, suggesting the possibility of focal areas of detachment prior to processing.
References:
- Albert DM, Phelps PO, Surapaneni KR, Thuro BA, MD, Potter HAD, Ikeda A, Teixeira LBC, Dubielzig, RR. The Significance of the Discordant Occurrence of Lens Tumors in Humans versus Other Species. Ophthalmology; 2015122(9):1765-1770.
- Beckwith-Cohen B, Teixeira LBC, Dubielzig RR. Presumed primary intraocular chondrosarcoma in cats. J Vet Diag Invest. 2014; 26(5):664-668.
- Dubielzig RR, Everitt J, Shadduck JA, Albert DM. Clinical and morphologic features of post-traumatic ocular sarcomas in cats. Vet Pathol. 1990; 27:62-65.
- Dubielzig RR. Non-surgical trauma. In: Dubielzig RR, Ketring KL, McLellan GJ, Albert DM, ed. Veterinary Ocular Pathology: A Comparative Review. Philadelphia, PA: Saunders Elsevier; 2010:81-114.
- Durham AC, Popovitch CA, Goldschmidt MH. Feline chondrosarcoma: a retrospective study of 67 cats (1987-2005). J Am Anim Hosp Assoc. 2008; 44:124-130.
- George DP, Zamber RW. Chondrosarcoma metastatic to the eye. Arch Ophthalmol 1996; 114:349-351.
- Rozeman LB, Cleton-Jansen AM, Hogendoorn PC. Pathology of primary malignant bone and cartilage tumours. Int Orthop. 2006; 30:437-444.
- Rodrigues EF, Jr., Ribeiro AP, Perlmann E, et al. Metastatic intraocular chondrosarcoma in a dog. Vet Ophthalmol. 2009; 12:254-258.
- Tay CY, Sathiyanathan P, Chu SW, et al. Identification and characterization of mesenchymal stem cells derived from the trabecular meshwork of the human eye. Stem Cells Dev. 2012; 21:1381-1390.
- Thompson KG, Dittmer KE. Tumors of Bone. In: Meuten DJ, ed, Tumors of Domestic Animals, 5th Ames IA, Wiley-Blackwell, 2017: 848-849.
- Zeiss CJ, Johnson EM, Dubielzig RR. Feline intraocular tumors may arise from transformation of lens epithelium. Vet Pathol. 2003; 40:355-362.