Signalment:
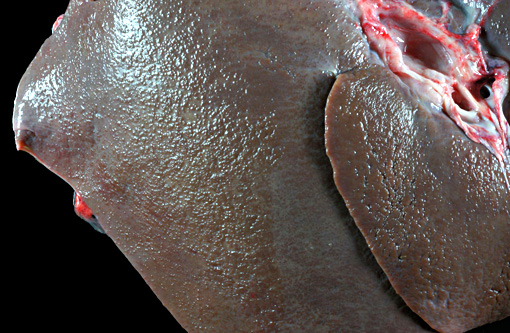
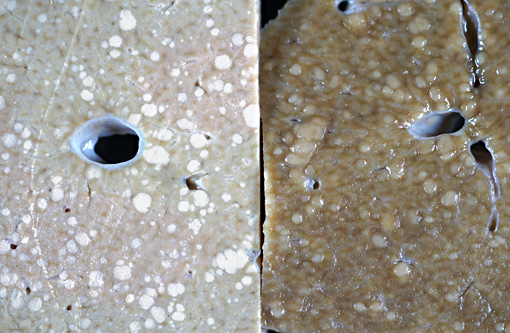
Gross Description:
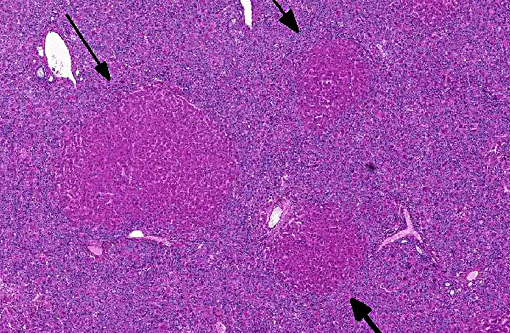
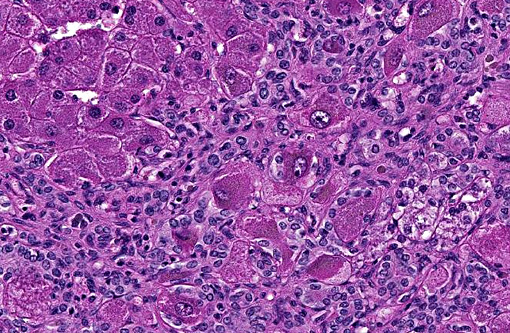
Histopathologic Description:
Morphologic Diagnosis:
Lab Results:
Condition:
Contributor Comment:
The most important genera are Senecio, Cynoglossum, Amsinckia, Crotalaria, Echium, Trichodesma, and Heliotropium. In New Zealand, PA toxicity in grazing animals is mostly associated with ragwort (Senecio jacobaea) poisoning. While ragwort is considered to be the most likely toxicant in this case, other possible causes of PA toxicity in New Zealand include: German ivy (Senecio mikanoides), groundsel (Senecio vulgaris), Patersons curse (Echium plantagineum), vipers bugloss (E. vulgare), borage (Borago officinalis) and comfrey (Symphytum spp. & hybrids).(1)
Pyrrolizidinosis is usually a chronic disease but acute toxicity may occur due to the variations in PAs content that can occur between seasons and years.(1) PAs are hepatotoxic, carcinogenic, genotoxic, teratogenic and sometimes pneumotoxic.(7)
PA exists in the plant in two molecular forms: the hydrophilic nontoxic N-oxide (amine-oxide) and the lipophilic pro-toxic free or tertiary bases (retronecine, heliotridine and otonecine). Toxicity occurs when these free bases are converted into highly reactive and unstable alkylating pyrroles or pyrrolic derivatives by liver microsomal enzymes (cytochrome P-450 monooxygenases mainly CYP3A and CPY2B6). Subsequently the C-7 or C-9 position of the pyrrolic ring system becomes highly electrophilic and capable of binding to proteins and/or nucleic acids, leading to altered cell function and cell damage or death.(3) Individual animal variation in toxicity of PAs is mediated by the activity of the estereases that detoxify the alkylating pyrroles. Different PAs have different toxicity due to differences in total alkaloid content, structural features of the amino alcohol and the presence of other substitutions on the chemical ring that modify the rate and extent of the toxicity. Toxicity of PAs is due to necrosis, antimitotic action (crosslinks with DNA and inhibits mitosis with concomitant formation of megalocytes) and vascular damage mainly in the liver. Some alkylating pyrroles can escape the liver and reach the lung damaging capillaries and resulting in acute pulmonary edema and hydrothorax. Renal damage is also reported.(1)
Ragwort (tansy ragwort, Saint James wort) is a biennial, perennial or annual weed with a diffuse root system. The alkaloids of ragwort include jacobine (major alkaloid), jaconine, jacoline, jacozine, senecionine and seneciphylline. All parts of the plants are toxic and animals normally eat the plant in small quantities either inadvertently or when forced due to lack of other food.(1)
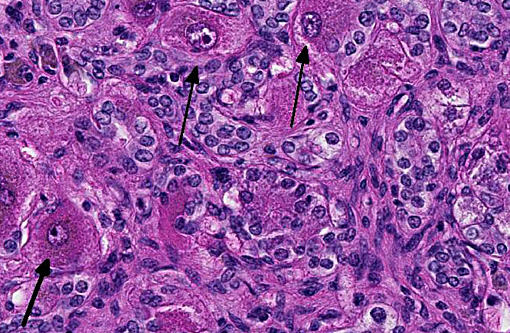
Pigs, horses, cattle, sheep, goats and chickens can be affected.(1,2) In humans, certain liver and other diseases have been attributed to the consumption of foods and herbal medicines prepared from pyrrolizidine alkaloid-containing plants.(6) Clinical signs in horses can be non-specific such as anorexia, weight loss, and diarrhea, photosensitization, icterus, or related to hepatic encephalopathy (depression, ataxia, circling, head pressing, blindness, collapse, coma and death).(2) There are three common histological patterns associated with pyrrolizidine poisoning: acute periacinar zonal necrosis, hepatic atrophy with formation of regenerative nodules, and atrophy and fibrosis without nodular regeneration. Megalocytes are usually most prominent in the second histological pattern. Megalocytosis is a progressive enlargement of liver cells to up to three times the normal diameter, with a proportionate increase in nuclear diameter. These are believed to be morphologically and functionally viable hypertrophic cells that are incapable of division due to the potent antimitotic action of the pyrrolizidine alkaloids. Some enlarged nuclei have cytoplasmic invaginations that can become entrapped as intranuclear inclusions.(6)
JPC Diagnosis:
Conference Comment:
The contributor discusses the three types of patterns of hepatic lesions associated with PAs. The acute form results from ingestion of a large quantity of toxin, as can occur in starving animals grazing drought stricken pasture. In the second form, likely present in the current case, repetitive prolonged exposure leads to the hepatic atrophy with megalocytosis. The third form, which lacks regenerative nodules, is due to prolonged exposure specifically to Heliotropium spp.(4)
The biliary hyperplasia is dramatic in this case, and often occurs in PA toxicosis. While this biliary reaction is commonly associated with bile duct obstructions or local portal inflammation and fibrosis, it is suspected to occur in toxicity cases such as PA, phomoposin, and aflatoxin due to sustained regenerative stimulus from an incapacitated atrophic liver.(4)
References:
1. Chambers, P. Poisonous plants of New Zealand. 2014 15/05/2014]; Available from: http://calve/pharm/toxSite/poisonplants/index.html.
2. Gava, A. and C.S. Barros, Senecio spp. poisoning of horses in southern Brazil. Pesquisa Veterin+�-�ria Brasileira, 1997. 17(1): p. 36-40.
3. Molyneux, R., et al., Pyrrolizidine alkaloid toxicity in livestock: a paradigm for human poisoning? Food Additives & Contaminants: Part A, 2011. 28(3): p. 293-307.
4. Stalker MJ, Hayes MA. Liver and biliary system. In: Maxie MG, ed. Jubb, Kennedy, and Palmers Pathology of Domestic Animals. Vol 2. 5th ed. Philadelphia, PA: Elsevier Saunders; 2007:373-376.
5. Stegelmeier BL, Edgar JA, Colegate SM, et al. Pyrrolizidine alkaloid plants, metabolism and toxicity. J Nat Toxins. 1999;8(1):95-116.Â
6. Svoboda, D., J. Reddy, and S. Bunyaratvej, Hepatic Megalocytosis in Chronic Lasiocarpine Poisoning: Some Functional Studies. The American Journal of Pathology, 1971. 65(2): p. 399.
7. Wiedenfeld, H., Plants containing pyrrolizidine alkaloids: toxicity and problems. Food Additives & Contaminants: Part A, 2011. 28(3): p. 282-292.