Signalment:
Male, spontaneously hypertensive (SH) rat (
Rattus norvegicus).The rat was found to be dorsally recumbent, with head tilting to the right and nystagmus of the left eye.
Gross Description:
Pale, finely pitted kidneys.
Histopathologic Description:
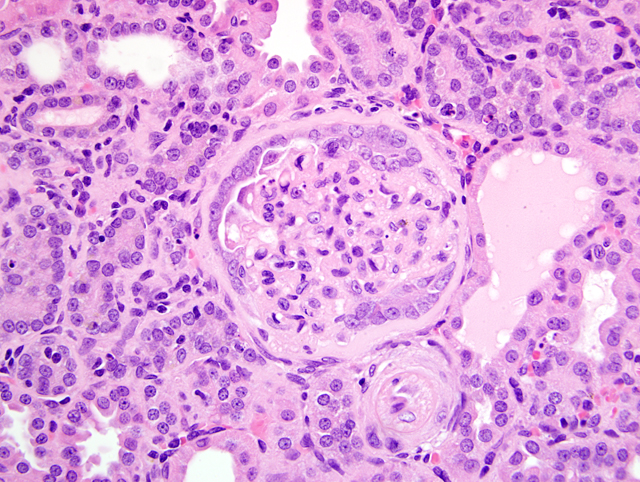
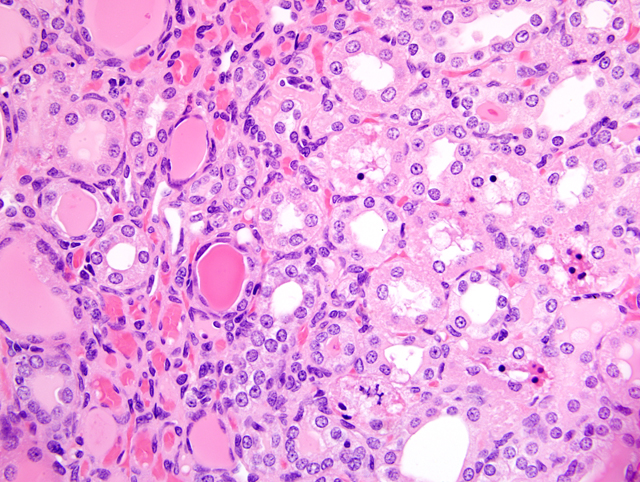
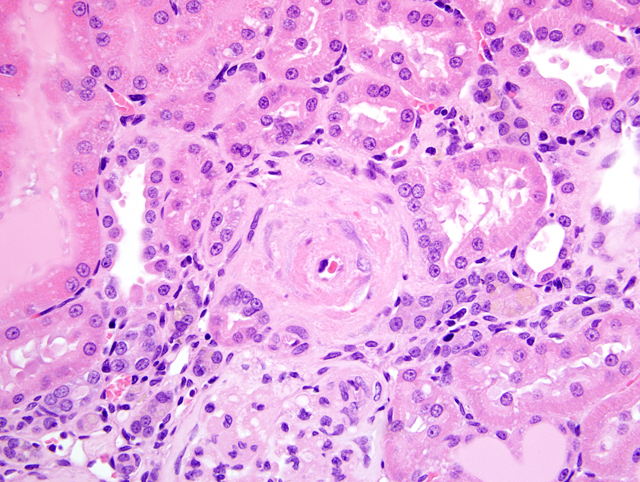
The renal capsular surface is diffusely undulant, with multiple shallow cortical indentations and multifocal tubular ectasia. Cortical indentations are often associated with perivascular cortical interstitial expansion and basophilia that correlate to an inflammatory cellular infiltrate comprised of small to moderate numbers of lymphocytes and macrophages, and a few light yellow brown pigment-laden macrophages (presumed hemosiderophages). The leukocytic infiltrate is multifocally accompanied by enhanced prominence of blood vessels, occasional hemorrhage, minimal to mild fibrosis, and separation/compression/loss of renal tubules. Renal proximal tubules and collecting ducts are multifocally ectatic with proteinaceous casts. In lesser affected tubules, the epithelium contains modest numbers of hyaline droplets. Other tubules exhibit sloughing of renal tubular epithelium (degeneration), presence of cellular and karyorrhectic debris (necrosis) and cellular and granular casts. Many scattered renal tubules exhibit tubular basophilia (regeneration). A few tubules also have thickened basement membranes. Glomeruli in markedly affected areas are often closely arranged due to tubular drop out. Multifocally, basement membranes of glomerular tufts and capsules are thickened and fibrotic (glomerulosclerosis). Multiple arcuate and/or interlobular arteries in the renal cortex exhibit reduction of vascular lumen, intimal deposits and medial smooth muscle hyperplasia with occasional degeneration of medial smooth muscle. The pelvic lamina propria has multifocal infiltrates of lymphocytes.
Morphologic Diagnosis:
Nephropathy, chronic, marked, with multifocal lymphohistiocytic interstitial nephritis, glomerular and tubular basement membrane thickening, glomerulosclerosis, tubular degeneration/necrosis/regeneration, tubular ectasia, casts and hyaline droplets, and arterial smooth muscle hyperplasia and degeneration.
Condition:
Chronic progressive nephropathy; arterial smooth muscle hyperplasia and degeneration
Contributor Comment:
The case represents chronic progressive nephropathy (CPN) in rats, which is common in old, male, Sprague-Dawley or Fischer 344 rats fed high protein diets.(4) CPN is a combination of both degenerative and proliferative lesions, and basophilic tubules are considered to be an early lesion in this nephropathy.(2,3) In chronic studies, the proliferative components of CPN may need to be discriminated from pre-neoplastic proliferative changes.(2) Degenerative lesions similar to those observed in this case could result from infections, degenerative nephrosis or toxic insults. However, the inciting factor is often difficult to discern by histologic evaluation. The vascular changes observed in this case may be related to the rat being spontaneously hypertensive and may have contributed to the development of the renal lesions.(1,2) Vascular lesions are typically not described in cases of CPN. Hence, in other strains, polyarteritis nodosa would be a good differential.
JPC Diagnosis:
1. Kidney: Glomerulonephropathy, diffuse, chronic, marked, characterized by glomerular sclerosis and synechia, tubular atrophy, degeneration, necrosis, regeneration, ectasia, and proteinosis, and interstitial fibrosis and nephritis.
2. Kidney, cortex: Arteriolosclerosis, proliferative, multifocal, moderate, with medial degeneration and necrosis, and smooth muscle hyperplasia.
Conference Comment:
In addition to the lesions described above, several conference participants slides contained fibrinoid necrosis in multiple affected vessels. As mentioned by the contributor, vascular lesions are not typical of CPN, so their presence should raise the index of suspicion for another cause, such as strain phenotype. Recognized risk factors for the development of CPN in rats include the following:(3)
- ) Age: greater than 12 months
- ) Sex: male
- ) Strain: Sprague-Dawley or Fischer 344
- ) Diet: high protein and/or total caloric intake
- ) Mesangial IgM deposition
- ) Elevated prolactin levels
Conference participants discussed the importance of CPN as a potential confounder in laboratory investigations in general, and in two-year carcinogenicity assessments in particular, as alluded to by the contributor. The earliest changes, i.e. basophilic tubules with thickened basement membranes, may be present in kidneys of rats as young as two months of age. In advanced stages, the proliferative lesions of CPN may be difficult to distinguish from preneoplastic hyperplastic lesions, termed atypical tubule hyperplasia (ATH). Specific criteria to make this important distinction have been proposed, and are summarized in the table below:(2)
| | Simple Tubule Hyperplasia | Atypical Tubule Hyperplasia |
| Significance |
Compensatory regenerative response to cellular injury and loss |
Preneoplastic developmental stage in a continuum with renal tubule adenoma/carcinoma |
| Cytoplasm |
Basophilic |
Mostly basophilic "glassy" cytoplasm; esoniophilic, clear, chromophobic, and oncocytic forms also described |
| Histomorphology |
Thickened basement membrane; increased number of epithelial cells; extends laterally but not generally inward beyond the single layer of tubule lining |
Proliferation beyond a single layer of tubular epithelium to form a solid tubule profile; expands into surrounding matrix and partially surrounded by rim of connective tissue cells; transition to early adenoma when proliferation extends beyond the nephron integrity |
References:
1. Feld LG, Van Liew JB, Galaske RG, Boylan JW: Selectivity of renal injury and proteinuria in the spontaneously hypertensive rat. Kidney Int
12:332-343, 1977
2. Hard GC, Seely JC: Recommendations for the interpretation of renal tubule proliferative lesions occurring in rat kidneys with advanced chronic progressive nephropathy (CPN). Toxicol Pathol
33:641-649, 2005
3. Hill GS: Hypertensive nephrosclerosis. Curr Opin Nephrol Hypertens
17:266-270, 2008
4. Percy DH, Barthold SW: Pathology of Laboratory Rodents and Rabbits, 3rd ed., pp. 161-162. Blackwell Publishing, Ames, IA, 2007