Joint Pathology Center
Veterinary Pathology Services
Wednesday Slide Conference
2017-2018
Conference 19
April 4th, 2018
CASE IV: 4079-14 (JPC 4048433).
Signalment: Neonatal, male and female, Dorper (Ovis aires), ovine.
History: Of 36 pregnant ewes, 14 have lambed in the last week. The lambs (2) with goiters died within 10 minutes of birth. The normal lamb also died after birth. Examination of the ewe reveals a possible small thyroid swelling. All lambs were frozen before submission.
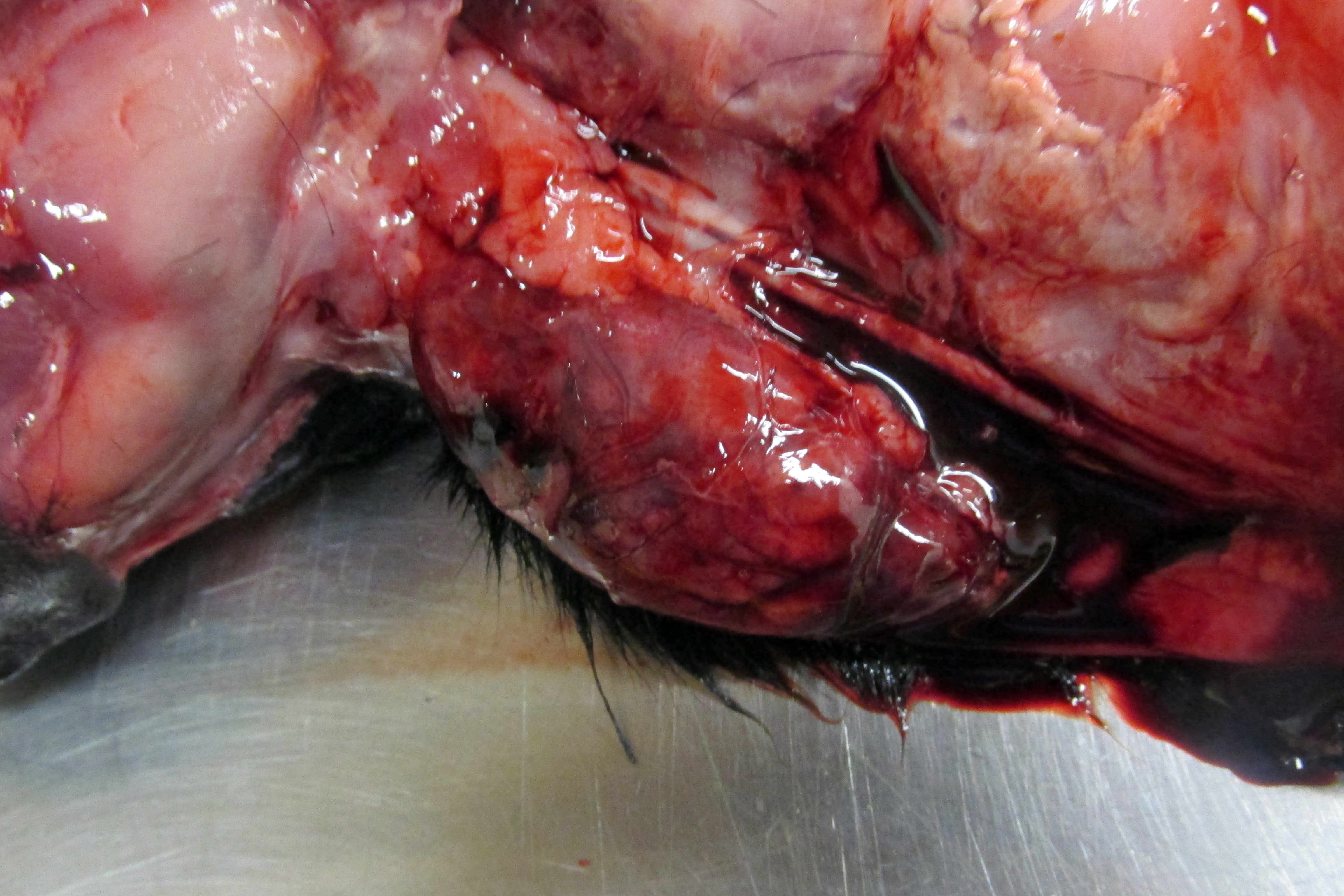
Gross Pathology: Examined at necropsy are two term affected lambs and an unaffected lamb. The lambs had been frozen and thawed prior to examination. The affected lambs externally have a large subcutaneous bulge in their anterior neck behind the larynx. The affected lambs are a female of body weight 2.2 kg and crown-rump length 31.1 cm and a male weighing 2.7 kg and having a crown rump length of 35.3 cm. The female affected lamb has a brachygnathic mandible. The unaffected lamb is a female of body weight 2.15kg and crown-rump length of 33.5 cm.
The unaffected lamb has a well-developed thick hair coat all over its body. The female affected lamb has no hair on the anterior aspects of the lower extremities, ventral abdomen or trunk. The only relatively normal hair is present on the neck, although there is also some hair on the posterior aspects of the legs below the elbow and stifle. The male affected lamb has similar alopecia on the anterior aspects of the front and rear legs, ventral body, and particularly scrotum, and a sparse, poorly developed hair coat on the trunk, especially on the posterior trunk. Hair on the head and neck is more normal.
The female affected lamb has enlarged thyroids that are 7 cm long X 2.5 cm in greatest diameter and weigh 26.6 grams. The male’s thyroids are 7 cm long X 3 cm in greatest diameter and weigh 2.15 grams. The enlarged thyroids are dark red in color and fleshy in texture. The left thyroid of the female contained a simple well defined cyst of 0.8 cm diameter located in the middle of the gland. The thyroids of the unaffected lamb are 2 X 0.7 cm and weigh 0.6 grams.
No visceral abnormalities are noted, including in the adrenals or pituitary. The eyes and brain are proportionally of normal size. The white matter of the spinal cord is a similar intensity of white between the affected and unaffected lambs.
Laboratory Results (clinical pathology, microbiology, PCR, ELISA, etc.): None provided.
Microscopic Description:
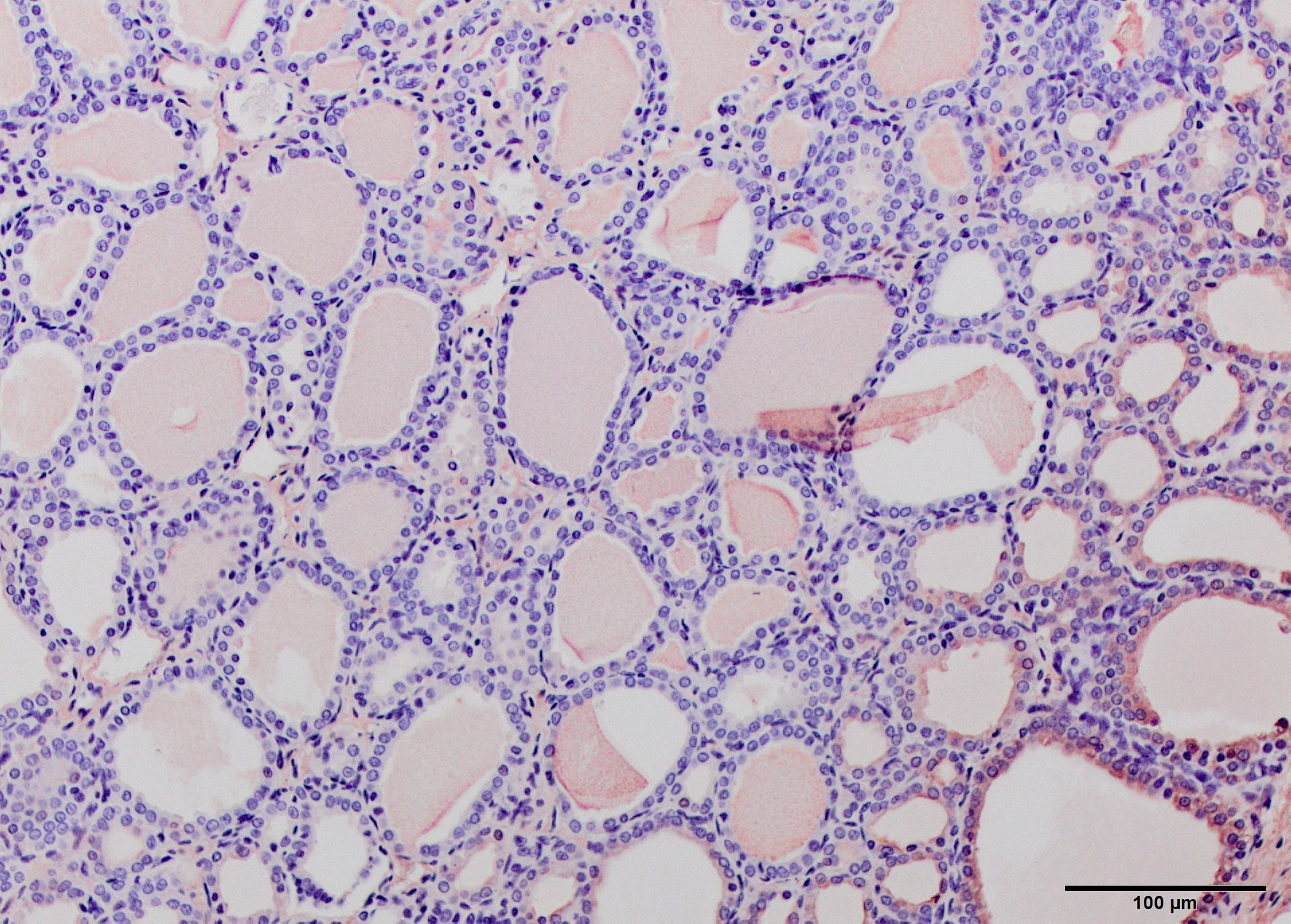
Thyroid gland: The thyroid follicles in both affected lambs are enlarged, sometimes spanning several 4X fields. The colloid has decreased eosinophilia and increased granularity. The follicular cells are frequently detached, although they remain at the periphery of follicles (freezing artifact). Interstitial cells are difficult to appreciate. The thyroid from the unaffected lamb has isomorphic follicles containing moderately eosinophilic colloid and a layer of cuboidal cells lining each. There is mild to moderate sloughing of colloidal epithelium (freezing artifact).
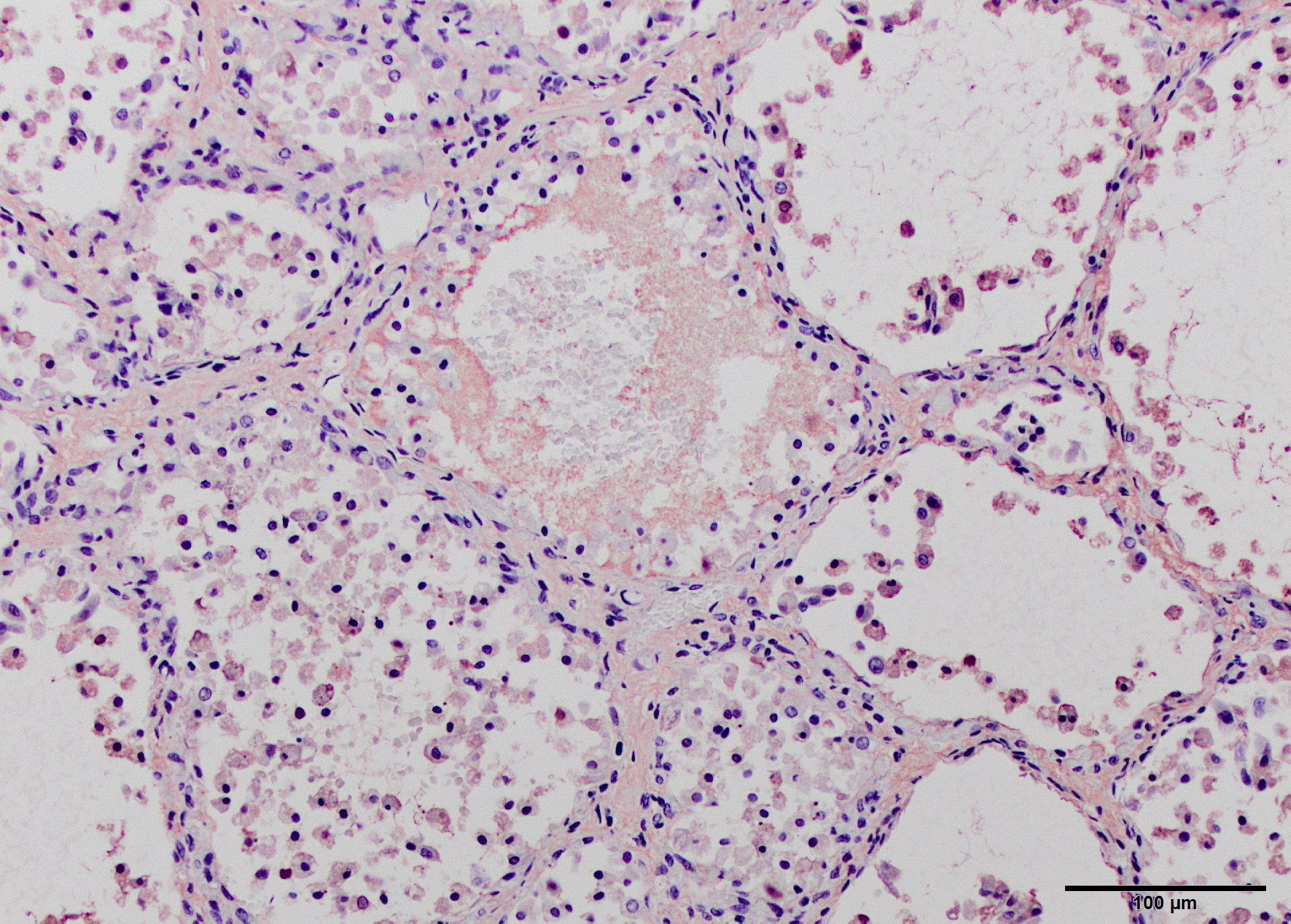
Skin: Affected lambs have reduced numbers of hairs protruding from the follicles. In some affected sections the epidermis is thinner and the hairs are farther apart, with mild myxedema of the deep dermis. In some sections there is basophilic ground substance consistent with myxedema in the upper dermis as well.
Contributor’s Morphologic Diagnosis:
Colloid goiter
Epidermal atrophy with alopecia
Contributor’s Comment: This case demonstrates congenital goiter and the alopecic skin disease that often is present.
Goiter or thyroid hyperplasia can result from multiple mechanisms: iodine deficiency, ingestion of goitrogenic compounds that interfere with thyroxine production, excess iodide and genetic mechanisms that interfere with biosynthesis of thyroid hormones.2 All of these etiologies result in activation of the hypothalamus as a result of low T3 and T4, with the result of increasing TSH. Common goitrogenic plants include thiouracil, sulfonamide and plants of the Brassica group. Offspring of deficient dams develop severe bilateral thyroid enlargement as in this case, with hyperplasia and hypertrophy of thyroid follicular cells and enlargement of interstitial blood vessels. Increased iodide blocks release of T3 and T4, resulting in enhanced TSH secretion.2
Hypothyroidism in animals, including sheep, and people can result in abortions, stillbirths and congenital abnormalities.2
In hyperplastic goiter, follicles vary in size; colloid is hypereosinophilic and may be vacuolated. Follicles are lined by one or more layers of epithelium, with small basal nuclei. Finger-like projections of cytoplasm may protrude into the follicle lumens. In these lambs, the colloid was pale and several large cysts were present. Following correction of the problem, the gland may become pale, as reduced TSH reduce endocytic resorption of colloid and condition is called colloid goiter.4
Thyroxine or T4 is the major product of the thyroid gland but is not active as an effective transcription factor. T4 must be deiodinated to T3 before it can bind to the nuclear receptor and the reaction regulated the bioavailability. Sulfation may also play a role in fetal thryoxine metabolism, as the addition of sulfate accelerates deiodination to inactive metabolites. Sulfation is upregulated during gestation in sheep during the last trimester and may regulate the supply of fetal T3 and facilitate maternal-fetal exchange. Iodine is concentrated by the placenta during fetal life.7 Glucuronidation of thyroxine occurs in liver and precedes biliary-fecal excretion. Stimulation of glucuronidation by various drugs can produce goiter in rats, but not humans.7
Congenital dyshormonogenetic goiter is inherited as an autosomal recessive trait in Corriedale, Dorset Horn, Merino and Romney sheep,3,5 Afrikaner cattle, and dwarf Saanen goats. Dorset horn sheep form part of the Dorper lineage. Inheritance is believed to be autosomal recessive in sheep. The most obvious changes in these sheep, besides thyroid enlargement, were abnormalities of the skin. Affected fetuses have abnormal hair coat, myxedema of the subcutis, weakness, and most die after birth. Thyroid follicles are described as collapsed due to lack of colloid,2 because there is increased endocytic activity and diminished ability to synthesize thyroglobulin. Iodine uptake is increased but blood T3 and T4 are low. The antibody used to stain for thyroglobulin was not optimized for sheep, but there was at least some staining of affected lambs’ thyroids. Unfortunately freezing and thawing of the tissue caused considerable artifact, which may have interfered with staining.
Under long term TSH stimulation, albumin and other proteins are iodinated by the thyroid. Iodine supplements restore normal thyroid hormone levels in affected sheep, even though thyroglobulin is absent. However, affected offspring die shortly after birth. Thyroglobulin RNA transcripts are incorrectly processed and no full-length protein results, yet the product is immunoreactive with anti-thyroglobulin polyclonal antibodies3 and IHC may not be a definitive differentiating test.
Few studies have been done on the histogenesis of fetal skin lesions during maternal hypothyroidism. Primary changes in rat skin include a significant decrease in epidermal thickness and reduction of hair follicle numbers.1 In addition, there is increased laminin deposition in the dermis and particularly the basement membrane.1 Laminin is important in connecting the dermis and epidermis. Hypothyroid rat pups developed increased laminin by 10 days of age. Number of hair follicles decreased and myxedema is present as in the skin of these lambs. Laminin is important to hair follicle development; T3 increases hair follicle survival in vivo considerably.
JPC Diagnosis: 1. Thyroid gland, follicular epithelium: Hyperplasia, diffuse, severe, Dorper (Ovis aires), ovine.
- Haired skin, superficial dermis: Myxedema, diffuse, moderate.
Conference Comment: Synthesis of thyroid hormone is unique among the other endocrine organs because hormone assembly occurs extracellularly within the lumen of the thyroid follicle. Iodide ions (I-) are collected from plasma by follicular cells, transported to the follicular lumen, and oxidized to iodine (I2). Thyroglobulin, a high-molecular-weight glycoprotein, is synthesized by follicular cells and contains tyrosine, which is an essential component of thyroid hormones and aids in their assembly as follows: Iodine binds tyrosyl residues in thyroglobulin to form monoiodotyrosin (MIT) followed by diiodotyrosine (DIT) which are coupled together to form T4 and T3 which is secreted by the thyroid gland in response to the hypothalamic-pituitary-thyroid axis (HPTA). The hypothalamus initiates the process by secreting thyrotropin-releasing hormone (TRH) which acts on the pituitary which releases thyroid stimulating hormone (TSH). TSH stimulates secretion of T3 and T4 from thyroid follicles. T3 and T4 act as a negative feedback mechanism to inhibit TSH release from the pituitary and induce somatostatin release from the hypothalamus which also inhibits TSH release from the pituitary. Additionally, T4 is converted to T3 within the pituitary gland and hypothalamus.6
Non-neoplastic and noninflammatory hyperplasia of the thyroid gland is termed “goiter” and is due to several pathogenic mechanisms: iodine deficiency or excess, goitrogenic compounds that interfere with thyroid hormone synthesis, and genetic enzyme defects in thyroid hormone synthesis. It is interesting that both deficiency of and excess iodine result in goiter. This is because iodine is required for synthesis of thyroid hormones, but, conversely, excess iodine interferes with fusion of colloid droplets and lysosomal bodies, blocking the release of thyroid hormones.6 The rest of these pathogenic mechanisms are described in detail by the contributor.
Newborns with goiter have unique gross characteristics such as: myxedema, alopecia, swollen tongue and laryngeal edema. The latter often contribute to death in newborns with goiter due to asphyxia and suffocation. The effect on the dam is often minimal except for prolonged gestation, dystocia, and retained placenta on occasion.6
True diffuse goiter must be distinguished from nodular hyperplasia, which is a fairly common finding in older horses, cats and dogs, appearing grossly as variably sized white nodules. In most animals, these nodules are not hormonally active, except in cats where they are typically functional.6
The diffuse myxedema within the superficial dermis is prominent in the submitted sections of skin from the affected animal. Evaluation of hair follicles in the absence of age-matched control or the unaffected lamb proved more problematic for attendees. While there are some focal areas in which hair follicles appear decreased in number, follicles do not show obvious signs of hypoplasia.
Contributing Institution:
Veterinary Medical Diagnostic Lab
University of Missouri
www.VMDL.missouri.edu
References:
- Amerion M, Tahajjodi S, Hushmand Z, et al. The effect of maternal thyroid disorders (hypothyroidism and hyperthyroidism) during pregnancy and lactation on skin development in Wister rat newborns. Iranian J Basic Med Sci. 2012;16:665-674.
- Capen CC. Endocrine Glands. In: Maxie MG, ed. Jubb, Kennedy, and Palmer’s Pathology of Domestic Animals. Vol. 3. 5th ed. St. Louis, MO: Elsevier-Saunders; 2007:389-393.
- Falconer IR, Roitt IM, Seamark RF, et al. Studies on congenitally goitrous sheep. Biochem J. 1970;117:417-424.
- Hetzel BS, Mano MT. A review of experimental studies on iodine deficiency during fetal development. J Nutrition. 1988;119:145-151.
- Jones BR, Greenway RM; Jolly RD, et al. A defect in thyroglobulin synthesis in an inherited ovine goiter: possible neonatal respiratory dist4ress syndrome. NZ Vet J. 1986;34:145-148.
- Rosol TJ, Grone A. Endocrine glands. In: Maxie MG, ed. Jubb, Kennedy, and Palmer’s Pathology of Domestic Animals. 3. 6th ed. St. Louis, MO: Elsevier; 2016:310-326.
- WuS-y, Green WL, Huang W-s, et al. Alternate pathways of thyroid hormone metabolism. Thyroid. 2006;15:943-958.